Lower Back Physical Therapy in Fort Myers, FL – Causes, Symptoms, & Treatment
Get Rid of That Pesky Lower Back Pain for Good with Lower Back Pain Physical Therapy in Fort Myers, FL…
Lower back pain is a widespread issue that can significantly affect your quality of life. Fortunately, physical therapy offers an effective approach to address the root causes of this pain and provide lasting relief. In this comprehensive guide, we will explore various lower back conditions and how skilled physical therapists can effectively treat them.
Understanding Physical Therapy for Lower Back Pain

Physical therapy is widely acknowledged as one of the most effective methods for managing lower back pain and injuries. Unlike short-term solutions that merely mask symptoms, physical therapy targets the underlying causes of pain, reducing the likelihood of recurring issues and long-term suffering. Scientific research supports the effectiveness of physical therapy for lower back pain. A study involving over 753,000 patients between the ages of 18 and 60 found that those who received early physical therapy treatment for back pain incurred significantly lower medical costs compared to those who delayed treatment (Childs et al., 2015). This emphasizes the financial benefits of early intervention. For individuals with chronic lower back pain lasting over 12 weeks, physical therapy remains the primary treatment option. Recent scientific reports classify physical therapy as a “first-line” treatment for chronic back pain due to its remarkable effectiveness and safety (Shipton, 2018).
Physical therapy treatments are tailored to address each patient’s specific needs and symptoms. Skilled physical therapists prescribe stretching, strengthening exercises, and other techniques to alleviate pain and promote healing. The specific exercises and treatments are based on the patient’s condition and medical history. Typically, patients attend physical therapy sessions once or twice a week, with the treatment plan adjusted as needed based on progress.
What Physical Therapy Entails
Physical therapy, administered by Doctors of Physical Therapy (DPT), focuses on the evaluation and conservative management of spine disorders. Unlike other medical practitioners, DPTs refrain from prescribing painkillers or invasive procedures to merely alleviate pain temporarily. Instead, they embark on a holistic approach to treat the root cause of the pain, thus preventing its recurrence.
The core elements of a physical therapy treatment plan may encompass stretching exercises, strengthening exercises, massage and foam rolling therapy, and heat/cold therapy.

However, the specific exercises and treatments employed vary according to the patient’s condition and medical history.
Initial sessions with a physical therapist often occur once or twice a week, with adjustments made to the treatment plan as necessary. These skilled professionals may also incorporate manual therapy and spinal manipulation techniques as part of the treatment process. During these hands-on approaches, the therapist targets specific points, mobilizes joints, and enhances circulation, all of which contribute to pain relief and long-term healing.
It’s important to note that manual therapy and spinal manipulation administered by physical therapists are considered safer alternatives to chiropractic care, which may employ more aggressive methods with a higher risk of injury.
Preparing for Your Physical Therapy Session
Before attending your initial physical therapy session, it’s beneficial to assess your lower back pain and share valuable observations with your therapist. Take note of factors such as what makes the pain better or worse, how long you’ve been experiencing it, and any previous treatments you’ve tried. Such information can guide your therapist to a more accurate diagnosis and treatment plan.
What Makes Your Pain Better or Worse?
Observe the following details:
-
Identify the circumstances that alleviate or exacerbate your back pain, such as sitting, standing, or sleeping. Your posture and age can significantly influence your lower back pain. Inadequate physical activity or excess weight can strain your back.
-
Consider underlying medical conditions. Diseases like cancer or arthritis, along with psychological conditions like anxiety and depression, can contribute to back pain.
-
Evaluate your lifting techniques. Proper lifting involves minimizing strain on your back by lifting from your legs, not your back. Poor lifting practices can lead to pain and injuries.
-
Note your smoking or nicotine product use. Nicotine products, especially through smoking, vaping, or e-cigarettes, can diminish blood flow to your spine, hindering nutrient delivery to your back discs and slowing the healing process. Nicotine can also exacerbate conditions such as Degenerative Disc Disease and increase the risk of osteoporosis.
A team of spine surgeons has noted that nicotine can also intensify Degenerative Disc Disease (when wear-and-tear of spinal discs cause pain) and increase the risk of osteoporosis (a condition that decreases bone density and can contribute to fractures), (Spinasanta et al., 2019).
How long have you suffered the pain?
Additionally, relay how long you’ve been experiencing the pain, whether it falls under acute, sub-acute, or chronic since each require a different treatment plan.
- Acute Pain = pain that started within the past week
- Sub-acute pain = pain that you’ve had anywhere from a week to twelve weeks
- Chronic pain = pain that you’ve had for more than twelve weeks
What Treatments Have You Tried?
In discussing previous treatments you’ve attempted, include those that provided relief and those that did not, to avoid reiteration of ineffective methods.
The Physical Therapist’s Diagnostic Process
Your physical therapist will rely on your observations, a physical examination, and a comprehensive health history to determine the cause of your lower back pain. This multifaceted approach is essential for crafting an accurate diagnosis and identifying the root cause of your pain.
Here’s a breakdown of the diagnostic process:
Step 1: Initial Questions
The first step involves the therapist posing a series of questions related to your back pain, aimed at gathering essential information about your condition. These questions will encompass various aspects, such as your age, health-related habits, and the presence of specific symptoms like unexplained weight loss, muscle weakness, or sensory alterations.
The physical therapist may ask detailed questions like:
- “What factors seem to alleviate or exacerbate your back pain?”
- “How long have you been experiencing this pain?”
- “Can you identify a specific incident or mechanism that triggered the pain? Did it result from a sudden injury or accident, or has it developed gradually over time?”
- “What are your primary objectives or goals for treatment?”
- “Have you previously attempted any treatments for your condition?”
While these questions may appear trivial at first, they hold considerable importance as they aid the physical therapist in pinpointing the underlying causes of your pain and devising an optimal treatment strategy for its alleviation.
Step 2: Physical Examination
Following the initial questionnaire, your physical therapist proceeds with a thorough physical examination aimed at gaining a deeper understanding of the issues surrounding your lower back. This examination serves as a crucial step in establishing an accurate diagnosis and identifying the root cause of your pain.
Once the underlying cause is ascertained, your physical therapist will formulate a customized treatment plan designed to address the source of the problem, with the ultimate goal of providing long-term relief from your symptoms.
“Here at Back in Motion, we Fix the Cause — Not just the Symptoms”
Throughout the physical examination, your physical therapist may request you to undertake the following assessments:
Step 3: Range of Motion

A “range of motion” assessment is employed to gauge the extent of movement achievable around a particular joint or body segment. To maintain an optimal range of motion, it is essential for the joint or muscle to exhibit good flexibility. This evaluation may involve the use of a goniometer, a tool resembling a ruler, delicately placed against the patient’s body to measure the joint angles.
When the assessment indicates a “poor range of motion,” it signifies that the joint or muscle lacks flexibility, potentially leading to discomfort and impeding the patient’s recovery process. Fortunately, a physical therapist can collaborate with the patient to enhance their range of motion, ultimately enabling increased flexibility and expediting the recovery journey.
Step 4: Muscle Strength Test

During this evaluation, you’ll be instructed to contract your muscles while engaging in straightforward movements. Your physical therapist might request that you perform actions like pressing down on their hand with your leg or applying force to their hand using your quadriceps (the muscle group situated in front of the hamstrings).
Physical therapists utilize a muscle strength grading scale to assess the strength and functionality of your muscles. The outcomes of this assessment will offer valuable insights to your physical therapist, assisting them in determining the most suitable strengthening exercises tailored to your specific needs.
Step 4: Neurological Tests
Your Doctor of Physical Therapy will guide you through various neurological tests to ascertain if there is any nerve involvement in your condition. These assessments encompass a range of evaluations, including:
- Reflex Testing: To assess your reflexes.
- Sensation Evaluation: To determine any alterations in your sensory perception.
- Muscle Strength Assessment: To gauge the strength and functionality of your muscles.
- Neural Tension Tests: To check for any tension or pressure on the nerves.
These neurological tests are essential in helping your physical therapist understand the extent of nerve-related factors in your condition, enabling them to tailor your treatment plan accordingly.
Step 5: Cause Detection Test
In certain cases, pinpointing the exact cause of an injury or pain can be challenging, even after initial assessments. If the cause remains unclear during the initial evaluation, your physical therapist will develop a treatment plan based on available information about your condition.
Throughout the course of your physical therapy, your therapist will continuously gather more data and insights to better understand the underlying cause, and they will adjust your treatment plan accordingly.
For example, one common culprit of persistent and often misdiagnosed lower back pain is related to limitations in the adjacent joints, such as the thoracic spine and hips. When these areas are weak or tight, they can lead to excessive movement or compensation in the lower back. Your physical therapist will work to address these issues as they become clearer during your treatment.
Step 6: Functional Test
This phase of the evaluation focuses on your ability to carry out everyday tasks effectively and aims to uncover the underlying causes of pain or injury.
For example, a common functional test involves standing on one leg and bending down to reach the floor to pick up an object. This test provides valuable insights into your bending and back usage techniques.
Moreover, for runners experiencing lower back pain during running, a crucial aspect evaluated is hip extension, a motion necessary for running. Poor hip extension in runners is often linked to lower back pain.
These assessments gauge various factors such as coordination, muscular balance, flexibility, and strength, providing essential information about your progress during your physical therapy journey.
Lower Back Conditions That Your Doctor of Physical Therapy Treats & How They are Treated
Once your specific condition has been diagnosed, your physical therapist will formulate a customized plan that takes into account the nature and severity of your ailment, the unique elements associated with your condition (including your medical history and factors that exacerbate or alleviate your symptoms), and your lifestyle. Additionally, proficient physical therapists may employ hands-on manual techniques to improve your mobility and alleviate discomfort, encompassing methods like manual therapy, including myofascial release, and spinal manipulation. If you recognize the symptoms of any of these lower back conditions discussed below, then exploring how a physical therapist can address your specific condition is essential.
1. Herniated & Bulging Discs
Herniated and bulging discs, while sharing similar symptoms, have distinct underlying causes. These conditions typically arise due to factors such as poor posture, spinal hypermobility, and improper bending techniques.
A herniated disc occurs when the soft, gel-like interior of your spinal disc protrudes into the spinal canal. This displacement exerts pressure on neighboring nerves, resulting in pain, numbness, and tingling sensations that often radiate from your back down into your leg.
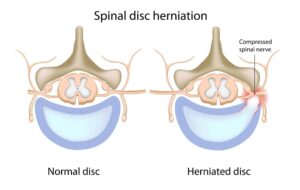
Conversely, a bulging disc manifests when a crack develops in the disc’s outer layer, causing it to change shape and protrude outward. This alteration can also create pressure on nearby nerves.
Signs & Symptoms of a Herniated Disc
Symptoms of a Herniated Disc encompass leg pain, often concentrated on one side of the body, numbness or tingling sensations in the lower extremity, unexplained muscle weakness, a burning sensation in the affected area, and worsened pain during bending or prolonged sitting.
Treatment of a Herniated Disc
In the treatment of a herniated disc, your physical therapist will concentrate on fortifying the affected region with tailored strengthening exercises. These exercises aim to reduce the herniation or bulge while facilitating the healing of the disc’s outer layer, known as the annulus.
Your Doctor of Physical Therapy may also explore the use of spinal traction, repetitive extension-based exercises, and positional distractions to alleviate pressure on the nerve root, ultimately alleviating your leg, buttocks, or thigh symptoms.

Once the pain and neurological symptoms have subsided from your leg, the treatment shifts towards disc recovery and an investigation into the root cause of the disc herniation. Factors such as spinal hypermobility, necessitating enhanced stability, or poor bending mechanics due to limited flexibility, will be considered in the design of a tailored treatment plan to address the herniated disc.
As your disc embarks on the healing process, your condition is expected to improve, leading to the gradual reduction of troublesome symptoms
2. Joint Stiffness
Joint stiffness can arise from various factors, including the natural wear and tear of joints over time, injuries, arthritis, or other medical conditions and diseases.
Signs & Symptoms of Lower Back Stiffness
Identifying the signs and symptoms of lower back stiffness can be crucial. These may encompass:
- Stiffness and pain upon waking
- Discomfort and stiffness after prolonged periods of lying and pain after lying, sitting, or standing still
- Reduced muscle flexibility
- Limited joint mobility
Treatment
Addressing joint stiffness and restricted mobility typically involves a comprehensive approach. Your skilled physical therapist will prioritize techniques such as:
- Mobilization exercises designed to enhance joint flexibility
- The use of heat to promote increased blood circulation to the affected joints
- Application of ice to alleviate inflammation
- Manual therapy to mobilize the joint and provide relief to the surrounding muscles
Furthermore, your Doctor of Physical Therapy will prescribe tailored exercises to specifically target and improve spinal mobility and overall range of motion. This holistic approach aims to alleviate joint stiffness, enhance flexibility, and promote your overall well-being.
3. Postural Lower Back Pain
As the name implies, one of the primary culprits behind postural lower back pain is poor posture. Incorrect standing, lifting, or sitting over extended periods can exert abnormal stress on the spine, potentially leading to structural changes in this vital area.
When left untreated, postural back pain can escalate, with many patients eventually developing conditions like bulging or herniated discs. Poor posture can fundamentally reshape the spine, potentially constricting blood vessels and nerves, ultimately triggering discomfort. This condition may also contribute to issues affecting your discs, joints, muscles, and ligaments.
Signs & Symptoms of Postural Lower Back Pain
Recognizing the signs and symptoms of postural lower back pain is critical, as they may include:
- Poor posture
- Muscle weakness or tightness
- Inadequate core stability
- Sedentary lifestyle
- Pain when sitting for prolonged periods
Treatment of Postural Lower Back Pain
Your dedicated physical therapist will begin by pinpointing the muscles responsible for your poor posture, tailoring specific strengthening exercises to address these areas. Once your postural muscles are reinforced, maintaining good posture becomes more manageable.
Additionally, your physical therapist will guide you on proper sitting techniques, as incorrect sitting can hinder the effectiveness of other treatments. Given that this condition is closely associated with poor posture, addressing sitting habits is crucial in preventing ongoing irritation of your lower back.
Over time, certain muscles may have tightened due to sustained poor posture. To counteract this, your physical therapist will prescribe exercises designed to enhance your flexibility, thereby reducing stiffness and pain. For example, prolonged sitting often leads to a rounded thoracic spine, which can heighten the risk of postural pain in the lower back.
In some cases, skilled physical therapists may incorporate manual therapy and spinal manipulation alongside other treatments. These manual techniques aim to improve circulation, loosen muscles, aid in muscle tissue repair, mobilize stiff joints, reduce inflammation, and enhance the function of nerves that may have been compressed due to poor posture.
4. Sacroiliac Joint Dysfunction
Sacroiliac Joint Dysfunction is a condition where the joint, whether hypermobile or hypomobile, may become inflamed, leading to lower back pain.
Various factors can contribute to this condition, including pregnancy and childbirth, weak muscles in the pelvis or lower back, scoliosis, leg length discrepancies, or previous lower back surgery.
Signs & Symptoms of SI Joint Pain
- Dull pain in the lower back
- Pain radiating into the buttocks and thigh
- Pain localized across the SI joint
- Pain experienced at the end ranges of motion or during prolonged sitting
- Poor stability in the lower back and pelvic region while sitting, standing, or exercising
- Hypermobility syndrome
Treatment of Sacroiliac Joint Dysfunction
When seeking treatment for Sacroiliac Joint Dysfunction, your physical therapist will first assess whether your condition is primarily due to hypermobility or hypomobility of the joint.
-
Hypermobility: If the condition results from joint hypermobility, your physical therapist will emphasize stability exercises to enhance the joint’s stability.
-
Hypomobility: In cases of joint hypomobility, manual therapy and spinal manipulation may be recommended to mobilize the joint. Additionally, a personalized treatment plan will be crafted, comprising stretching, strengthening, and aerobic exercises to alleviate stiffness and restore joint mobility.
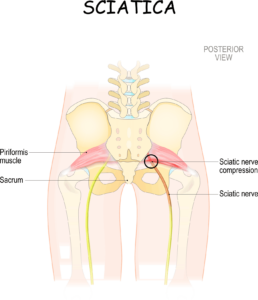
5. Sciatica
Sciatica is a condition characterized by lower back pain resulting from the irritation of the sciatic nerve. The sciatic nerve, the body’s largest nerve, originates in the lower back and extends through the buttock area. Its nerve endings travel down the lower limbs, which is why individuals often experience numbness or tingling in their leg when the nerve is irritated.
The most common cause of sciatic nerve irritation is the tightness, entrapment, or inflammation of the nerve at the piriformis muscle.
Signs & Symptoms of Sciatica
- Difficulty bending or sitting
- Numbness, tingling, or pain in the leg
- Pain with straightening the knee
- Muscle guarding of the piriformis muscle
- Pain during activities such as swinging a golf club or other sporting endeavors
- Difficulty sleeping
Treatment of Sciatica
When considering treatment for sciatica, your physical therapist will prescribe exercises and stretches specifically designed to enhance lower back flexibility and reduce stiffness. You may also be introduced to flossing exercises, which help stretch and move the sciatic nerve, providing relief.
In cases where flossing exercises fail to alleviate the issue, your physical therapist may employ myofascial release or the Active Release Technique to relax the piriformis muscle.
It’s important to note that if the pain is attributed to a herniated disc, treatment will be tailored to address this specific condition. Although herniated discs can mimic the symptoms of sciatica, their treatment differs significantly. This underscores the importance of consulting a healthcare professional for an accurate diagnosis.
Physical therapists who remain current with the latest treatment techniques may utilize methods such as manual therapy or myofascial release to relax tightened muscles and tissues, particularly in the piriformis muscle, providing effective relief for individuals experiencing sciatica.
6. Spinal Stenosis Treatment
Spinal stenosis is a medical condition characterized by the narrowing of spaces within the spine, resulting in increased pressure on the nerves that traverse through the spinal canal. This narrowing is typically due to the wear-and-tear of the discs, causing the canal where the nerves exit the spine to constrict.
Spinal stenosis primarily affects the lower back and neck regions, and individuals with this condition may experience pain in both areas. Additionally, it can lead to symptoms like tingling, numbness, or muscle weakness, which tend to worsen over time.
Signs & Symptoms of Spinal Stenosis
- Numbness or tingling in a foot or leg
- Issues related to walking and balance
- Lower back pain
- Lower back pain exacerbated by standing and walking and relieved by sitting
- Bowel or bladder dysfunction (in severe cases)
Treatment of Spinal Stenosis
It is imperative to seek treatment for spinal stenosis, as this condition can progress and give rise to more severe symptoms, including bowel or bladder dysfunction and, in severe cases, paralysis if left untreated.
Your physical therapist will employ a variety of techniques and exercises specifically tailored to your condition to alleviate the compression on the nerves within the spinal canal.
One often overlooked aspect of spinal stenosis treatment involves addressing the hip. Tightness in the front of the thigh can lead to excessive arching of the lower back as the spine compensates. This, in turn, further narrows the spinal canal. Therefore, an effective approach to treating spinal stenosis involves stretching the front of the hip.
In cases where muscle weakness is evident, your physical therapist will prescribe targeted exercises to bolster your strength. Those experiencing balance and coordination issues will be provided with exercises to enhance these skills.
Moreover, your physical therapist may offer manual therapy and a personalized stretching regimen to enhance spinal flexibility and mobilization. This approach can manually open the foramen, reducing pressure on the nerves and relieving discomfort associated with spinal stenosis.
More About Treatments For Lower Back Pain
In our discussion, we’ve highlighted the efficacy of manual treatments like “manual therapy,” “spinal manipulation,” “myofascial release,” and targeted exercises. These approaches, when applied by experienced physical therapists, have proven effective in addressing a wide range of lower back conditions.
It’s important to recognize that physical therapists often employ a combination of these manual treatments along with other therapeutic modalities. This multifaceted approach is designed to not only alleviate the symptoms but also target the root causes of your specific condition, ensuring comprehensive care.
However, it’s crucial to acknowledge that not all Doctors of Physical Therapy possess the qualifications and expertise to administer these specialized interventions and treatments. Therefore, it’s essential to choose your healthcare provider wisely to receive the most effective and appropriate care for your lower back ailment.
To gain a deeper understanding of each treatment type, continue reading as we delve into the specifics of these therapeutic approaches.
1) Manual Therapy
Manual therapy encompasses a set of techniques, including therapeutic massage and joint mobilization, aimed at reducing pain and enhancing mobility. During your session, your skilled physical therapist will employ hands-on methods to manipulate and apply pressure to specific joints and muscles.
You might also be guided through particular stretches while your physical therapist applies controlled pressure at specific points on your body. This intricate form of therapy contributes to your healing process by diminishing pain, boosting your range of motion, facilitating improved blood circulation, and alleviating muscle spasms.
2) Myofascial Release
Myofascial release is a specialized manual therapy technique that concentrates on targeting myofascial tissue. Myofascial tissue is a form of connective tissue responsible for supporting and safeguarding muscles and bones.
When your myofascial tissue becomes excessively tight, it can lead to discomfort and limited mobility in specific areas of your body, especially in the lower back. Physical therapists possess the expertise to alleviate tension in myofascial tissue through a distinctive massage technique.
It’s essential to note that not all physical therapists are proficient in manual therapy and myofascial release. Typically, it requires the skills of highly trained physical therapists to expedite a patient’s recovery using these methods.
Dr. Scott Gray and his team of experts are renowned in their respective fields, assisting patients in achieving relief through the application of manual therapy, myofascial release, and spinal manipulation. Feel free to reach out today to discover how our proficient team can help alleviate your lower back pain.
Ready To Get Started?
Don’t hesitate to initiate your journey toward relief. You can get in touch with us by clicking the link below or by directly calling us at 888-973-2899.
Lower back pain treatment in Fort Myers!
Manual therapy and myofascial release are valuable treatments that offer both immediate and long-term relief to individuals grappling with chronic and acute back pain. These therapeutic approaches can effectively address joint issues, muscle strains, back injuries, as well as conditions like herniated or bulging discs.
3) Spinal Manipulation
Spinal manipulation is a specialized technique effective in alleviating acute lower back pain (pain experienced within the first 0-4 days) and sub-acute lower back pain (pain experienced within 1-12 weeks). During this procedure, a qualified practitioner, such as a physical therapist, chiropractor, or medical doctor, employs their hands or a specialized tool to administer a controlled thrust to a joint within the spine.
This controlled thrust serves to enhance joint mobility beyond its natural capabilities. Consequently, spinal manipulation can improve both mobility and muscular functionality while mitigating pain.
It’s important to note that chiropractors sometimes adopt a more aggressive approach to spinal manipulation, potentially increasing the risk of side effects or unintended consequences. Fortunately, Doctors of Physical Therapy tend to adopt a more conservative approach, aiming to maximize the benefits while minimizing potential risks. This approach ensures a safer and more effective therapeutic experience.
#4 Specific & Custom Exercises
Just as with medication, exercise is a potent intervention. Whether you’re dealing with an illness or an urgent medical condition, the right dosage of a specific drug can either improve your health or exacerbate the issue.
When it comes to exercise, it’s no different. Exercise can be thought of as a type of “prescription,” and like any drug, too little or too much can yield adverse effects.
The same principle applies to the selection of exercises. Engaging in the wrong exercises can either improve your condition or worsen it.
This underscores the vital role of a knowledgeable Doctor of Physical Therapy in your treatment. These experts can precisely identify the nature of your lower back condition, recognizing that each ailment demands a tailored and precise treatment approach.
For example, if you’re dealing with a disc herniation, performing flexion exercises can exacerbate your lower back pain.
Likewise, administering spinal manipulation to a “hypermobile” patient can intensify their symptoms. This is why seeking the guidance of a skilled professional is of paramount importance in ensuring the right exercises are prescribed for your unique condition, thereby promoting a safe and effective path to recovery.
What Can you Do in the Meantime?
Rather than enduring discomfort until your scheduled appointment, there are several widely recommended back pain relief exercises and strategies suggested by physical therapists that you can try to initiate the process of recovery.
Should you experience exacerbation of your symptoms while implementing these suggestions or engaging in the provided back pain relief exercises, it’s essential to discontinue them. Make sure to communicate to your physical therapist which exercises have had an impact on your condition, whether positively or negatively. This information will contribute to a more accurate assessment and tailored treatment plan during your consultation.
Tip #1: Pay Attention to Posture
Your posture is a daily habit that can significantly impact your overall well-being. Poor posture can increase your vulnerability to fractures, injuries, and discomfort. Changing ingrained habits can be challenging, but making a conscious effort to maintain good posture while sitting, standing, or moving can help retrain your brain to automatically adopt a healthier posture.
What constitutes proper posture? To gain a sense of good posture, you can perform posture tests while sitting, standing, and walking:
Correct Sitting Posture

- Sit with your buttocks and back against the chair’s backrest, maintaining forward-facing alignment so that your ears are directly above your shoulders.
- Position your knees at or slightly below hip height, ensuring your feet are flat on the floor with ankles just in front of the knees.
- If your lower back doesn’t make contact with the chair’s backrest while maintaining an upright posture, you can place a rolled-up towel or a back-support pillow between the chair and the curve of your lower back.
Correct Standing Posture

- Stand with your feet shoulder-width apart, maintaining a slight bend in your knees, and face forward to align your ears over your shoulders.
- Imagine a straight line running down your body, connecting your head, shoulders, hips, knees, and feet. There should be a slight curve in your lower back and shoulder blades.
- You can assess your standing posture by standing against a wall with your heels about two inches away from it and your feet shoulder-width apart, knees slightly bent. Your head, shoulder blades, and buttocks should all make contact with the wall.
- Place your hand in the space between your lower back’s curve and the wall. This space should be roughly the thickness of your hand.
- If there’s more space than the width of your hand, engage your abdominal muscles to flatten the curve in your back until you attain the correct space.
- If you find yourself pushing too hard against your hand, create more space by arching your back slightly to achieve the right distance.
- If you struggle to position yourself correctly during the standing wall test, your physical therapist can assess your posture and provide tailored exercises to help you make the necessary adjustments.
Correct Walking Posture

- Ensure that your head, shoulders, hips, knees, and feet form a straight line at the center of your body as you walk.
- When swinging your arms forward, keep them close to your body and below chest height.
- Maintain relaxed shoulders and refrain from clenching your fists; instead, hold them gently in a slightly curled position, as if you were carrying a few potato chips.
By making a concerted effort to maintain proper posture, you can reduce the risk of various musculoskeletal issues and promote your overall well-being.
Tip #2 Reduce Your Phone Usage
If your phone usage mirrors the habits of many Americans, who spend approximately two hours daily staring at screens, it’s advisable to consider the following questions and take steps to improve your habits:
-
Can the activities I perform on my phone be done on a computer with a more ergonomic setup?
Evaluating whether you can transition certain phone tasks to a computer with a better ergonomic arrangement may help reduce strain on your neck and spine.
-
Am I frequently looking down or tilting my head forward when using my phone?
If you find that you often tilt your head forward or look down at your phone, it’s essential to acknowledge this habit and work on correcting it.
-
Am I taking regular breaks to move and stretch my body during extended phone use?
Maintaining mobility and preventing prolonged periods of phone use without breaks are essential for reducing strain on your muscles and maintaining good posture.
If you answered “yes” to any of these questions, it’s advisable to consider strategies to reduce your phone usage and improve your posture:
- Minimize phone usage: Limit the time spent on your phone, especially for activities that can be comfortably transitioned to a computer with a more ergonomic setup.
- Create a posture-friendly workspace: Ensure your workspace, including computer and phone setups, promotes good posture and minimizes head tilting or looking down.
- Avoid craning your head forward: Be mindful of your head position and make an effort to maintain a neutral and relaxed head posture when using your phone.
By addressing these considerations and implementing positive changes, you can reduce the risk of neck and back strain associated with excessive phone usage and maintain better posture.
Tip #3 Keep Moving!
When you remain sedentary, whether sitting or standing for extended periods, your muscles tend to tense up. Numerous scientific studies have consistently shown that incorporating movement breaks every 20 to 30 minutes, even during brief periods of sitting or standing, can significantly reduce discomfort and stiffness.
Moreover, there’s compelling scientific evidence highlighting the manifold health benefits of staying active and the adverse consequences of prolonged periods of inactivity. For instance, a recent study published in the Journal of the American College of Cardiology revealed a direct correlation between excessive sitting and an increased risk of mortality (Stamatakis, 2019).
By understanding the importance of regular movement and the potential health implications of remaining sedentary, you can be motivated to take short breaks, stretch, or engage in light physical activity throughout your day. These simple yet effective practices can help alleviate muscle tension, enhance overall well-being, and mitigate the risks associated with prolonged periods of inactivity.
Tip #4 Back Pain Relief Exercises
In the video provided below, you’ll discover a set of highly beneficial back pain relief exercises designed to assist you in managing your discomfort as you await your scheduled physical therapy appointment. The video is presented by Dr. Scott Gray, a seasoned expert in physical therapy, who offers clear and comprehensive guidance on the proper execution of each exercise.
These exercises are organized into three distinct categories, addressing specific types of lower back pain:
- Alleviating Pain from Prolonged Sitting
- Easing Pain Experienced while Standing or Walking
- Managing Discomfort During Physical Activity
By engaging with these exercises, you can proactively take steps to reduce your back pain and improve your overall comfort. Dr. Scott Gray’s expert instructions will ensure that you perform each exercise correctly and safely, optimizing their effectiveness in providing relief tailored to your specific pain triggers.
Give Your Back a Break — Back in Motion PT is Here to Treat Your Lower Back Pain
Are you in search of a highly skilled team of experts and a specialized lower back pain specialist in Fort Myers? Your quest ends here at Back in Motion Physical Therapy & Performance, where our expertise has successfully alleviated back pain for a wide range of individuals, from healthcare professionals to the Mayor of Fort Myers.
Back in Motion has been featured on renowned platforms such as NBC Sports, ABC, and DEW TOUR, and stands as the premier physical therapy clinic in Southwest Florida for addressing orthopedic, sports, and spine injuries.
Ready to experience the transformative effects of our proficient physical therapists in bidding farewell to your lower back pain? Get in touch with us directly at 888-973-2899.







