November 2024
Why You Still Have Lower Back Pain Even After Injections or Surgery?
A Personal Note from Dr.Scott:

What I’m Thankful For This Thanksgiving
As Thanksgiving approaches, I find it’s the perfect time to reflect on all the things I’m truly grateful for. It’s a tradition that dates back centuries to the Pilgrims and Native Americans, who shared a feast in the early 1600s to celebrate a successful harvest and express gratitude for the cooperation and abundance they had experienced despite many hardships. This spirit of thankfulness has carried through generations, reminding us to appreciate what we have in the present moment.
On a personal level, I’m incredibly thankful for my health—something I don’t take for granted. I’m also grateful for the freedom of speech that allows me to express my thoughts and ideas openly. My supportive wife has been my rock, and my kids constantly remind me how important it is to stay young at heart (and quick on my feet!).
Beyond family, I want to extend my deepest gratitude to our amazing customers and patients. Your trust allows us at Back In Motion to do what we love—helping you move better, feel stronger, and lead active lives. Your commitment to your health inspires our team every day, and we feel privileged to be part of your wellness journey.
Wishing you and your loved ones a Thanksgiving full of joy, good health, and cherished moments. Thank you for being part of our Back In Motion family!
Dedicated to Your Success,
Dr. Scott Gray
P.S. Remember, “fix the cause and not the symptom”.
Featured Article of the Month
Why You Still Have Lower Back Pain Even After Injections or Surgery
Lower back pain is one of the most common issues adults face today, and many turn to injections or even surgery as a last resort. Yet, despite undergoing these invasive treatments, some people still find themselves in pain, frustrated, and without long-term relief. If you’re one of those people, you’re not alone—and there’s a good reason why the pain persists.
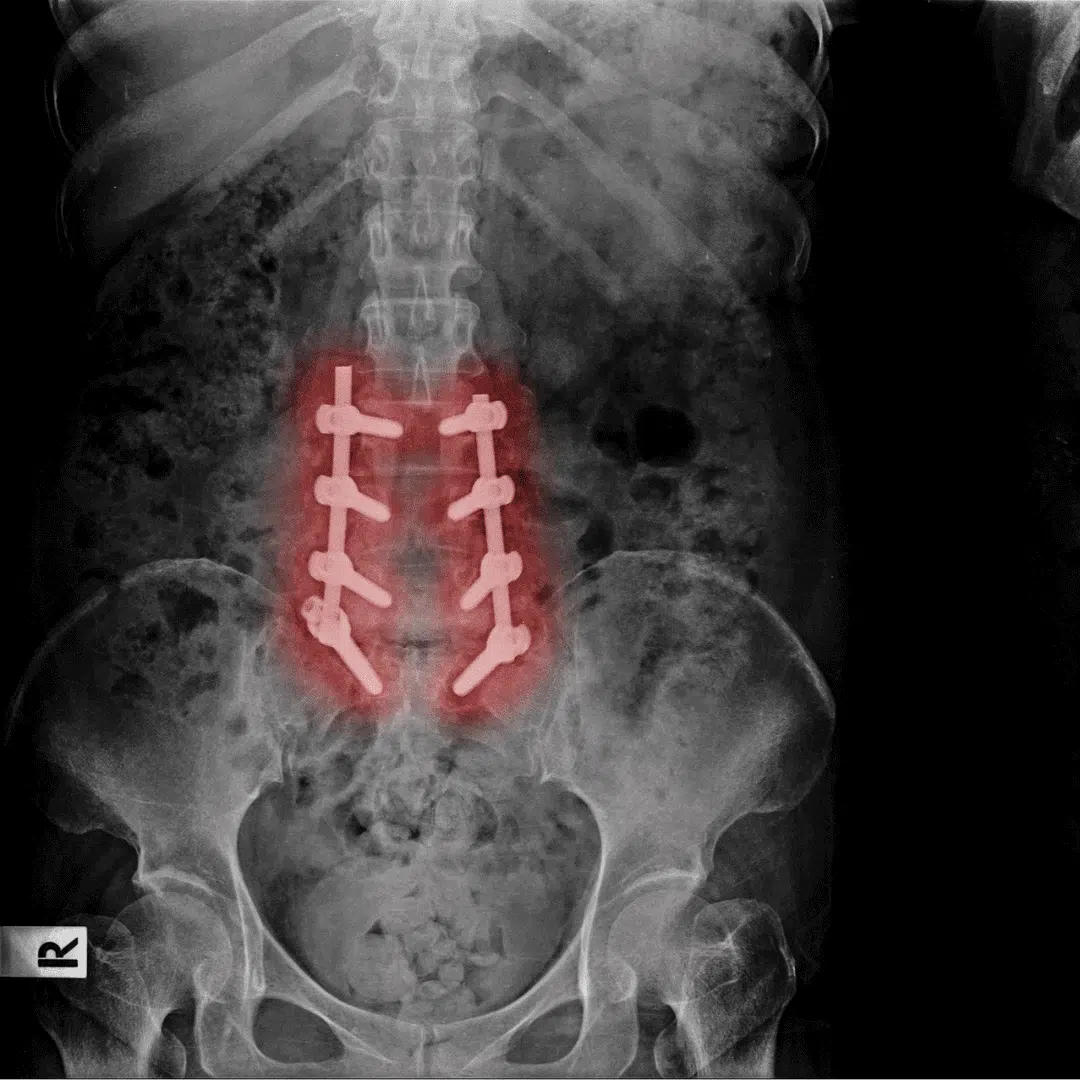
The truth is that imaging techniques like MRIs and X-rays often lead to false positives, showing abnormalities that might not be the actual source of your pain. The real issue for many individuals suffering from chronic lower back pain isn’t something a scan can easily pick up. Instead, the underlying cause may be lower back hypermobility—a condition that is rarely discussed, poorly understood, and often misdiagnosed, even by health professionals.
In this blog post, we’ll uncover why surgeries and injections often fail to provide lasting relief, explain what lower back hypermobility is, and discuss why so few practitioners can diagnose or treat it properly.
The Problem with Imaging: False Positives and Misdiagnosis
MRIs and X-rays are often the first step in diagnosing back pain, but they come with a major flaw—they frequently show abnormalities that may have nothing to do with your pain. Disc bulges, herniations, or degenerative changes are common findings in people with no symptoms at all. In fact, research shows that many adults over 40 who feel perfectly fine still have these abnormalities visible on imaging scans.
Surgeons often rely on imaging results to determine the need for surgery, but the images don’t tell the whole story. A bulging disc on an MRI might look like the culprit, but what if that bulge isn’t what’s causing your pain? This leads to surgeries on the wrong parts of the spine, leaving the actual issue untreated. The sad truth is that most cases of lower back pain—more than 99%—do not require surgery.
Why Surgery and Injections Fail
Many patients undergo back surgeries, such as spinal fusions or microdiscectomies, expecting the pain to disappear afterward. While some experience temporary relief, others find themselves back where they started—or worse. This is because surgery doesn’t always address the root cause of the problem.
In cases where injections are prescribed, they may reduce inflammation or numb the pain temporarily, but they don’t fix the underlying instability in your spine. Both injections and surgery can offer short-term relief, but without solving the real issue, the pain inevitably returns.
The Real Culprit: Lower Back Hypermobility
One of the most overlooked causes of lower back pain is hypermobility—a condition in which the joints in the spine move too much. Unlike a stiff joint, which is easy to spot on an X-ray or MRI, hypermobility is invisible on imaging. It occurs when the supporting structures—like muscles, ligaments, or the disc itself—are too weak or overstretched, allowing excess motion in the vertebrae. This extra movement irritates the surrounding tissues and leads to chronic pain.
What Is Lower Back Hypermobility?
In a healthy spine, the joints and surrounding tissues work together to allow just the right amount of movement. But with hypermobility, the joints become unstable, moving beyond their intended range. This instability can cause:
- Chronic muscle tightness as the body tries to compensate for the excess movement.
- Joint irritation from the vertebrae moving out of alignment repeatedly.
- Nerve sensitivity as the surrounding tissues become inflamed from overuse.
The pain caused by hypermobility often mimics other back issues, which is why it is frequently misdiagnosed. You might feel stiffness, spasms, or sharp pain, especially after standing, sitting, or bending for long periods. Yet, the real issue isn’t a stiff joint—it’s a joint that’s too loose.
Why Imaging Fails to Detect Hypermobility
MRIs, X-rays, and other imaging tools are excellent at identifying structural abnormalities—like herniated discs or fractures—but they cannot assess movement. That’s why lower back hypermobility often goes undiagnosed. Hypermobile joints only become a problem when they move, which means you need a functional assessment rather than a static image to identify them.
Unfortunately, most healthcare providers rely heavily on imaging. If your MRI looks normal, you might be told there’s “nothing wrong” with your back, even though the real problem lies in how your spine moves, not how it looks. This leads to patients being misdiagnosed or receiving treatments that don’t address the instability causing their pain.
Why Most Providers Miss the Diagnosis
Even beyond imaging issues, there’s another problem: most healthcare providers don’t know how to properly diagnose or treat hypermobility. Chiropractors, massage therapists, and even many physical therapists are trained to address stiff or restricted joints, but very few understand how to manage hypermobile joints.
The standard approach to treating back pain often involves:
- Chiropractic adjustments that restore motion but don’t address instability.
- Massage therapy that relaxes tight muscles but doesn’t stabilize the joint.
- Physical therapy that focuses on stretching, which can actually make hypermobility worse.
Without targeted treatment, these therapies offer temporary relief at best. Many providers overlook the need to stabilize the joints and strengthen the surrounding muscles, which is the key to managing hypermobility.
How to Treat Lower Back Hypermobility the Right Way
Treating lower back hypermobility requires a different approach than the typical back pain treatments. Instead of focusing on releasing tight muscles or stretching stiff joints, the goal is to increase stability in the spine. Here’s how it’s done:
1. Strengthening the Core Muscles:
A stable spine requires strong, coordinated muscles, especially in the core. The focus should be on deep stabilizers like the transverse abdominis and multifidus, not just the superficial abs.
2. Targeted Stabilization Exercises:
Exercises like bird-dogs, dead bugs, and planks—when done correctly—can improve spinal control and reduce excess motion in the joints.
3. Movement Retraining:
Many people with hypermobility need to relearn how to move properly. This includes training the body to engage the right muscles at the right time, preventing compensations that increase instability.
4. Avoiding Overstretching:
Stretching might feel good, but for hypermobile joints, it can make the problem worse. The focus should be on building strength and control, not flexibility.
5. Manual Therapy for Stability:
Some forms of manual therapy—like joint mobilizations or taping—can help provide temporary stability while you work on strengthening the spine.
Finding the Right Practitioner
Because lower back hypermobility is underdiagnosed and misunderstood, it’s essential to find a healthcare provider who understands how to assess and treat it. Look for:
- Specialized physical therapists who are experienced in functional assessments and stabilization training.
- Practitioners who avoid over-reliance on imaging and focus on movement-based assessments.
- A multidisciplinary approach that includes strength training, movement retraining, and manual therapy.
Conclusion: The Key to Lasting Relief
If you’ve had injections or surgery but still experience lower back pain, it’s time to consider that the real issue might be hypermobility. This invisible condition often goes undiagnosed, leaving patients stuck in a cycle of pain and ineffective treatments. The good news is that with the right approach—focused on stabilization rather than stretching or adjustments—lasting relief is possible.
At Back In Motion, we specialize in identifying and treating lower back hypermobility, helping our clients regain stability, strength, and control. If you’re ready to move beyond temporary fixes and find the root cause of your pain, we’re here to help.
Don’t let lower back pain hold you back any longer—schedule a consultation today and take the first step toward a pain-free life.
Oliver’s Healthy Recipe

Protein Pumpkin Pancakes with Cottage Cheese

These protein-packed pumpkin pancakes are the perfect way to fuel your fall mornings. Using cottage cheese as a base makes them fluffy, moist, and loaded with protein, keeping you satisfied throughout the day. Plus, they’re quick and easy to whip up!
Ingredients
- 1/2 cup cottage cheese
- 1/2 cup pumpkin puree
- 2 large eggs
- 1/2 cup oat flour (or blended oats)
- 1/2 teaspoon baking powder
- 1/2 teaspoon pumpkin pie spice
- 1/4 teaspoon cinnamon
- 1 teaspoon vanilla extract
- 1-2 tablespoons maple syrup (optional for sweetness)
- Pinch of salt
Ingredients
Optional Toppings:
- Greek yogurt
- Sliced bananas or berries
- Chopped nuts
- Drizzle of maple syrup or almond butter
Instructions:
- Blend the Ingredients:
In a blender or food processor, combine the cottage cheese, pumpkin puree, eggs, oat flour, baking powder, pumpkin pie spice, cinnamon, vanilla extract, maple syrup (if using), and a pinch of salt. Blend until smooth. - Preheat a Pan:
Heat a non-stick skillet or griddle over medium heat and lightly grease with a bit of butter or oil. - Cook the Pancakes:
Pour 1/4 cup of batter onto the skillet for each pancake. Cook for about 2-3 minutes until bubbles form on the surface, then flip and cook for another 1-2 minutes until golden brown. - Serve and Enjoy:
Top your pancakes with Greek yogurt, fruit, nuts, or a drizzle of maple syrup for extra flavor and nutrition.
These pancakes are great for meal prep too! Simply store leftovers in the fridge and reheat for a quick, protein-rich breakfast throughout the week.
Fitness Corner
Simple Ways to Stay Active During the Holidays – Even If You Don’t Have Time
The holidays are a whirlwind of family gatherings, shopping, cooking, and events, making it tough to stick to your usual fitness routine. It’s easy to feel overwhelmed, and back pain or other discomforts can make staying active feel impossible. But staying active doesn’t mean spending hours at the gym – small, simple movements can go a long way in keeping you healthy, mobile, and pain-free. Here are some practical ways to stay active during the holidays, even if your schedule feels packed.

1. Turn Holiday Tasks into Mini Workouts
Everyday holiday activities can double as opportunities to move. Use them to your advantage:
- Walking while shopping: Take the long route around the mall or store.
- Standing stretches while cooking: Stretch your legs, back, and arms between tasks.
- House cleaning for cardio: Play some music and use cleaning as a way to get your heart rate up.
Pro Tip: Break up sedentary time by setting a reminder to stand and stretch every 30-60 minutes.
2. Use 10-Minute Movement Breaks
Even short bursts of exercise can make a difference. If you can’t commit to long workouts, try 10-minute movement sessions:
- Bodyweight exercises: Do squats, lunges, or planks.
- Mini yoga session: Try gentle stretches to ease stiffness, especially if you experience back pain.
- Walk around the block: A quick walk can improve circulation and refresh your mind.
Consistency is key – even a few minutes a day helps maintain strength and mobility.
3. Choose Active Family Activities
Involve your family in physical activities that double as quality time:
- Holiday strolls: Go for a walk to look at lights or decorations.
- Play a family game outside: A game of tag or catch is a great way to get everyone moving.
- Dance parties at home: Put on festive music and dance together – it’s a fun way to stay active!
4. Stretch and Move Throughout the Day
Sitting for long periods during holiday meals, travel, or gatherings can stiffen your muscles, leading to back pain. Incorporate gentle stretches and movements throughout the day to avoid discomfort:
- Seated twists: Loosen up your lower back.
- Standing back extensions: Relieve back tension from sitting too long.
- Neck rolls: Keep your neck and shoulders relaxed during stressful moments.
5. Prioritize Movement Over Perfection
The holidays are about joy, not perfection. You don’t need to maintain your regular fitness routine to stay healthy – any movement counts. Focus on small wins, like choosing to walk instead of sitting or standing instead of lounging.
You’re Not Alone in the Struggle to Stay Active During the Holidays
We know how hard it can be to stay active with so much going on during the holiday season. The endless to-do lists, events, and family gatherings often leave little time or energy for movement. It’s easy to feel overwhelmed, but you’re not alone in this struggle – many people face the same challenge.
The good news? You don’t have to do it all yourself. Whether it’s finding the right exercises, staying consistent, or just knowing where to start, we’re here to help. At Back in Motion, we specialize in supporting people through the ups and downs of staying active, especially during the busiest times of the year.
It’s not about being perfect – it’s about finding small ways to move that fit your schedule and make you feel good. So, if you need a little extra guidance to keep moving forward, we’re here for you every step of the way. Let’s tackle the holidays together and make staying active simple and stress-free.
Spotlight on Dr. Sharon Sims: Over 40 Years of Dedication to Physical Therapy Excellence

Dr. Sharon Sims brings over four decades of expertise and passion to her practice. She began her journey as a Physical Therapist Assistant (PTA), laying a strong foundation in patient care and hands-on techniques. However, her dedication to her craft and her patients inspired her to pursue her Physical Therapy (PT) credentials, and for the past 30 years, she has been practicing as a PT, transforming countless lives along the way.
Dr. Sims is known for her holistic and highly effective approach to care. She incorporates manual therapy techniques, the renowned Gray Method™, and a focus on overall health and wellness to ensure her patients achieve long-lasting relief and a return to a pain-free, active lifestyle. Whether it’s addressing acute pain or helping patients improve their quality of life, Dr. Sims is committed to finding and fixing the root cause of problems—not just treating the symptoms.
Her wealth of experience and unwavering dedication make Dr. Sims a cherished member of our team and a trusted guide for anyone looking to restore their health and well-being.
Case Study
Case Study – How Lois Got Rid of Her Lower Back Pain with the Gray Method™ After Suffering for Two Years
How Lois Overcame Persistent Lower Back Pain with the Gray Method™
For years, Lois struggled with chronic lower back pain that interfered with her daily life. Every attempt to manage it—through medications, physical therapy, and even injections—seemed to offer only temporary relief. Frustrated and exhausted, Lois began to wonder if she’d ever be free from the pain that was holding her back from the life she loved.
But everything changed when Lois discovered the Gray Method™
The Frustration of Temporary Solutions
Like many people dealing with chronic pain, Lois had tried nearly every treatment option available. She’d visited numerous doctors, who often prescribed medication to mask the pain, and tried various therapies aimed at temporary relief. Despite her efforts, the pain kept coming back.
Lois began to feel discouraged, worrying that her lower back pain was something she’d have to live with for the rest of her life.
Finding the Gray Method™: A New Hope
When Lois heard about the Gray Method™, she was intrigued. The Gray Method™ is a unique approach to treating pain that focuses on identifying and addressing the root cause, rather than just managing symptoms. Developed by experts who understand that each body is different, the Gray Method™ centers on a customized approach, combining detailed assessments with tailored exercises to deliver lasting relief.
Unlike her previous treatments, the Gray Method™ gave Lois hope that she could finally understand why her pain kept returning—and how to address it for good.
A Customized Assessment to Find the Real Cause
The first step of the Gray Method™ was an in-depth assessment. Lois’s therapist took the time to understand her history, pain patterns, and lifestyle. Through careful analysis, they uncovered an issue that had been overlooked in previous treatments: lumbar hypermobility.
Lumbar hypermobility is a condition where certain joints in the lower back are overly flexible, which can lead to instability, inflammation, and chronic pain. This underlying cause hadn’t been detected in standard imaging, yet it was the key to Lois’s ongoing discomfort.
With this new understanding of her condition, Lois felt empowered and hopeful—she was finally addressing the cause, not just masking the symptoms.
A Tailored Treatment Plan
With the root cause identified, the Gray Method™ team developed a customized treatment plan specifically for Lois. Her plan included targeted exercises designed to strengthen the muscles around her lower back, stabilize her joints, and prevent future pain.
One of the biggest advantages of the Gray Method™ is its emphasis on safe, science-backed exercises that promote healing without aggravating the body. Lois’s therapist guided her through each movement, ensuring proper form and gradually building her strength and stability.
The Results: A Life Free from Lower Back Pain
After just a few weeks of following her personalized treatment plan, Lois began to notice significant improvements. Her pain levels decreased, her mobility improved, and she finally felt in control of her body again. By sticking with the exercises and adjustments recommended in the Gray Method™, Lois was able to return to the activities she loved without fear of pain.
Today, Lois lives an active, pain-free life, thanks to the Gray Method™.
The Gray Method™ Difference
For Lois, the Gray Method™ was more than just a treatment—it was a journey to understanding her body and reclaiming her freedom. By focusing on the root cause and providing individualized care, the Gray Method™ gave Lois the tools she needed to overcome chronic pain and take control of her health.
If you’re struggling with persistent lower back pain, consider the Gray Method™. It’s a safe, effective approach that addresses the underlying causes of pain, empowering you to live the life you deserve—free from pain and limitations.
Are you ready to start your journey to lasting relief? Contact us today to learn more about how the Gray Method™ can help you.
Testimonials

“I’m a little apprehensive about driving from Naples to Fort Myers, just physical therapy several times a week, but I’m glad I did. The outcome has been absolutely spectacular!
“

“I really like that you were more focused on getting me back in the gym because you knew that was really important to me.”