The Great Plantar Fasciitis Debate: Why Walking Boots & Cortisone Injections Rarely Fix the Problem (And What Really Does)
If you’ve been struggling with plantar fasciitis, chances are you’ve already heard the typical recommendations: “Wear a walking boot for a few weeks.” Or maybe, “Let’s try a cortisone injection to calm the inflammation.”
At first, these options sound promising. They seem quick. They sound medical. And they may even give you some temporary relief.
But here’s the uncomfortable truth: neither a boot nor an injection addresses the real problem—and that’s exactly why plantar fasciitis so often lingers or comes roaring back.
So today, let’s debate it.
We’ll compare the “quick-fix” approaches versus what actually works long-term—so you can make an informed decision about how you want to heal.
Side 1: The Case for Walking Boots & Cortisone Injections
Let’s be fair. Walking boots and cortisone injections are popular for a reason.
- Walking Boots:
The logic here is simple—if you immobilize the foot, you reduce stress on the fascia, giving it “time to heal.” - Cortisone Injections:
These powerful anti-inflammatory shots reduce pain and swelling quickly. They can give short-term relief that feels like a miracle, especially if you’ve been hobbling out of bed in the morning for months.
So yes—they can help you feel better. But only in the short run.
The Problems With These “Solutions”
1. They Don’t Fix the Cause
Plantar fasciitis isn’t just “inflammation.” It’s usually caused by mechanical overload—too much stress on the plantar fascia due to tight calves, limited ankle mobility, weak stabilizing muscles, or faulty foot mechanics (like overpronation or oversupination).
- A walking boot doesn’t fix mobility, strength, or foot mechanics.
- A cortisone injection doesn’t change how your body moves.
So when you go back to walking, running, or exercising—the same forces that caused the problem are still there.
2. Risk of Making Things Worse
- Walking boots can actually weaken muscles and create stiffness in the ankle. Many patients end up with more problems after weeks in a boot.
- Cortisone injections can temporarily weaken the tissue, and in some cases, have been linked to plantar fascia rupture—a painful complication that can take months to recover from.
3. They Create Dependency
Because they only mask symptoms, you may find yourself repeating them: another injection, another period in the boot, another cycle of frustration.
That’s not healing—that’s management.
Side 2: The Case for Fixing the Root Cause
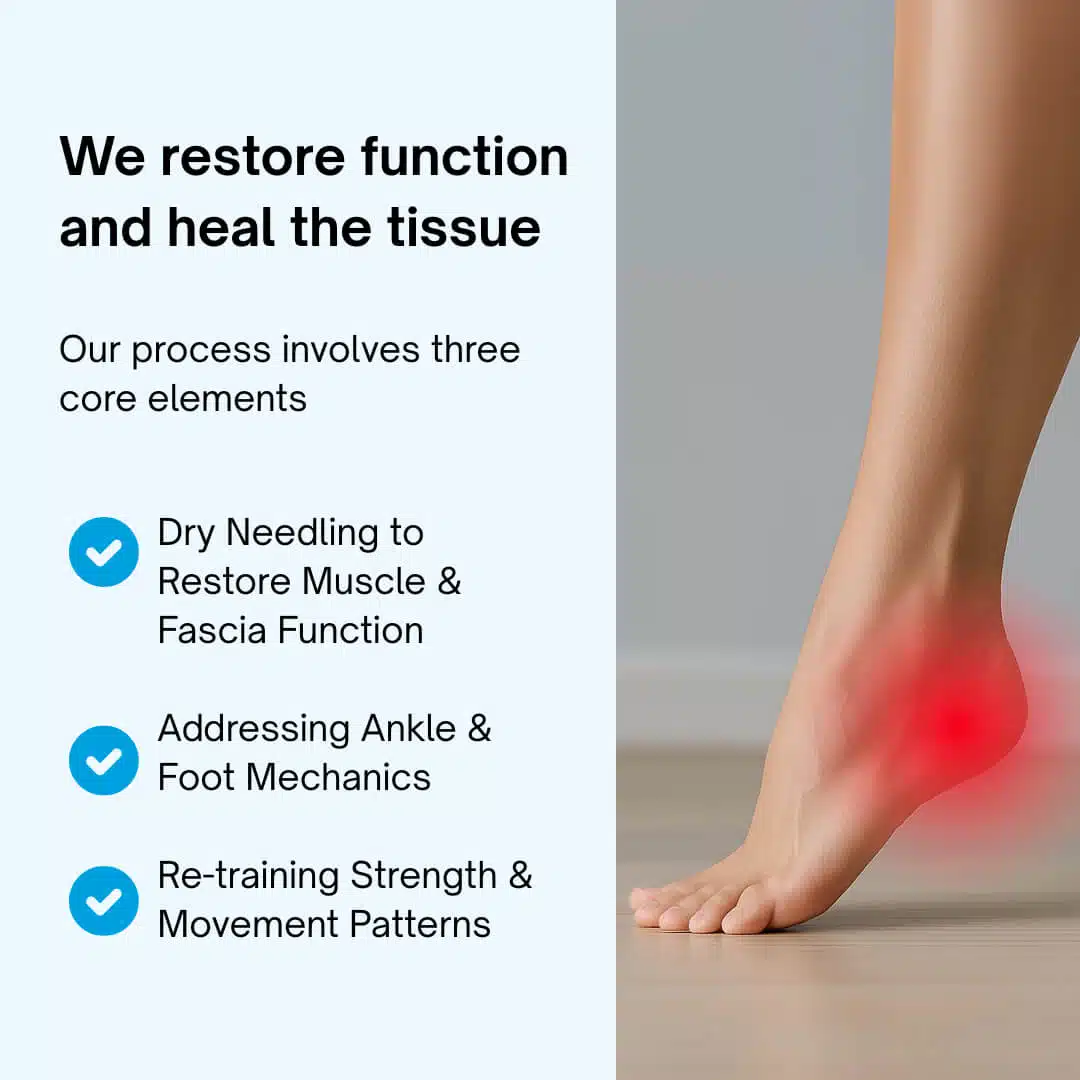
At our clinic, we take a completely different approach. Instead of masking symptoms, we restore function and heal the tissue so you can get back to activity without fear of the pain returning.
Our process involves three core elements:
- Dry Needling to Restore Muscle & Fascia Function
- Addressing Ankle & Foot Mechanics
- Re-training Strength & Movement Patterns
Let’s break it down.
Step 1: Dry Needling the True Pain Generators
Most people think plantar fasciitis is just about the plantar fascia itself. But what we see clinically is that certain muscles deep in the foot often drive the pain.
- Medial Calcaneal Tubercle: This is where the plantar fascia attaches. By dry needling this area, we can release tension, increase blood flow, and stimulate a true healing response.
- Flexor Digitorum Brevis (FDB): This muscle sits right under the plantar fascia and is frequently overloaded when the fascia is irritated. Needling here restores its function and reduces strain on the fascia itself.
- Quadratus Plantae (QP): This small but powerful muscle helps align the pull of the flexor digitorum longus. When it’s tight or dysfunctional, it contributes to foot fatigue and chronic heel pain.
By targeting these overlooked muscles, dry needling helps break the pain cycle and restore normal mechanics at the source.
Why this works better than injections: Instead of suppressing inflammation, dry needling stimulates controlled healing. It tells the body: “Hey, repair this tissue properly.” That’s the opposite of masking the problem.
Step 2: Restoring Ankle Mobility
Plantar fasciitis rarely happens in isolation. One of the biggest contributors? Stiff ankles.
If your ankle can’t bend (limited dorsiflexion), every step puts more load on your plantar fascia. Over time, that irritation adds up to pain.
That’s why we:
- Mobilize the ankle joint to restore normal motion
- Stretch and release tight calf muscles
- Re-train proper gait mechanics so the fascia isn’t overloaded
Why this matters: You can needle the fascia all day, but if the ankle is still locked up, the problem will just come back. Mobility is non-negotiable.
Step 3: Correcting Foot Mechanics (Pronation & Supination)
Another often-ignored factor is how your foot moves when it hits the ground.
- Overpronation (rolling in too much) flattens the arch and overstretches the fascia.
- Oversupination (not rolling in enough) creates a rigid, high-impact landing that strains the fascia.
We assess each patient’s foot mechanics and correct them with:
- Targeted strengthening of the intrinsic foot muscles
- Corrective exercises for the hips and knees (since they influence foot position)
- In some cases, customized orthotics to provide support while we retrain the body
Why this works: Instead of blaming your fascia, we fix how the whole chain above it works. The result? Lasting change.
The Real Debate: Quick Fix vs. True Fix
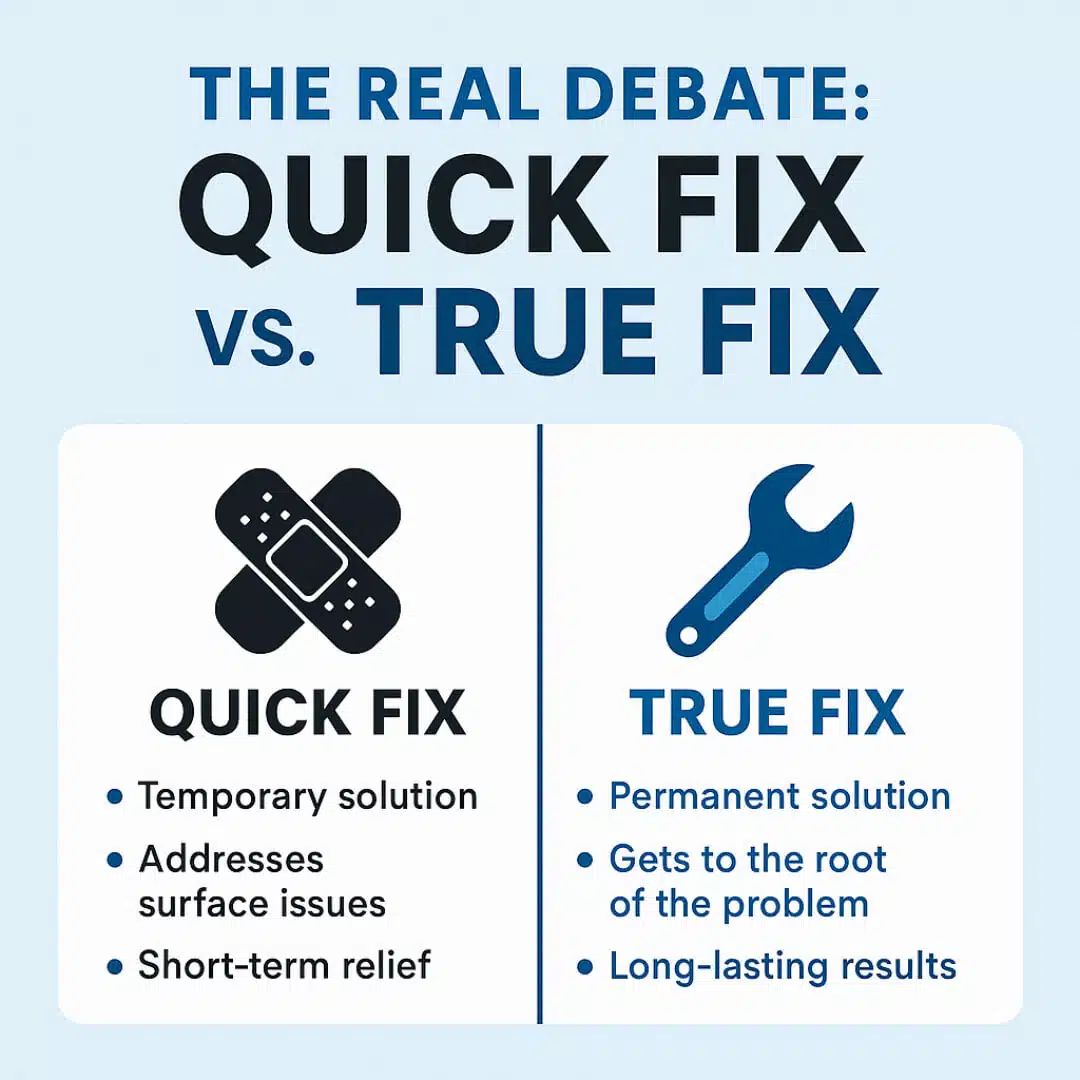
So let’s put it head to head.
Walking Boot / Cortisone Injection
Masks pain temporarily
Doesn’t improve function
Risk of side effects / setbacks
Relies on rest
Problem often returns
Dry Needling + Mobility + Mechanics Approach
Treats the actual cause of pain
Restores muscle, fascia, and joint function
Stimulates natural healing
Gets you back to activity faster
Long-term relief and prevention
It’s not even close.
A Real-World Example
I once treated a patient who had been through two cortisone injections and six weeks in a boot. Each time, she felt a little better—until she started walking again.
Then the stabbing heel pain returned.
When she came to us, we needled her medial calcaneal tubercle, FDB, and QP. We mobilized her ankle and corrected her excessive pronation with exercises. Within four weeks, she was walking pain-free. Within eight, she was back to running.
Her words: “I wish someone had told me this was possible before I wasted months in a boot.”
Why Most Clinics Don’t Treat It This Way
The unfortunate reality is that many clinics focus on symptom relief, not cause correction. Injections and boots are quick to prescribe, require little follow-up, and fit a traditional medical model.
But true healing takes more than a prescription—it takes a customized, hands-on approach. That’s exactly what makes our clinic different.
The Bottom Line
Walking boots and cortisone injections aren’t evil—they just aren’t the best solution. They may give you a few weeks of relief, but they rarely solve the problem.
If you’re tired of waking up with stabbing heel pain, skipping workouts, or planning your day around when your foot will hurt less, it’s time to stop debating short-term fixes.
Instead, focus on what actually heals:
- Dry needling the true pain generators (medial calcaneal tubercle, FDB, QP)
- Restoring ankle mobility
- Correcting faulty foot mechanics
That’s how you get rid of plantar fasciitis once and for all—and that’s why this debate, for me, isn’t even close.