5 Hidden Reasons Why Sciatica Occurs (That Most People Miss)
If you’ve been told “it’s just aging” or you’ve been stretching your hamstrings for weeks with little relief, you’re not alone. Sciatica isn’t one problem; it’s a pattern—usually a mix of mechanics, habits, and overload that irritates the nerve along its path. Below are five under-the-radar drivers I see every week in clinic, plus simple ways to start turning the ship.
1) Overuse of the Hamstrings (because the quads and glutes are under-doing their job)
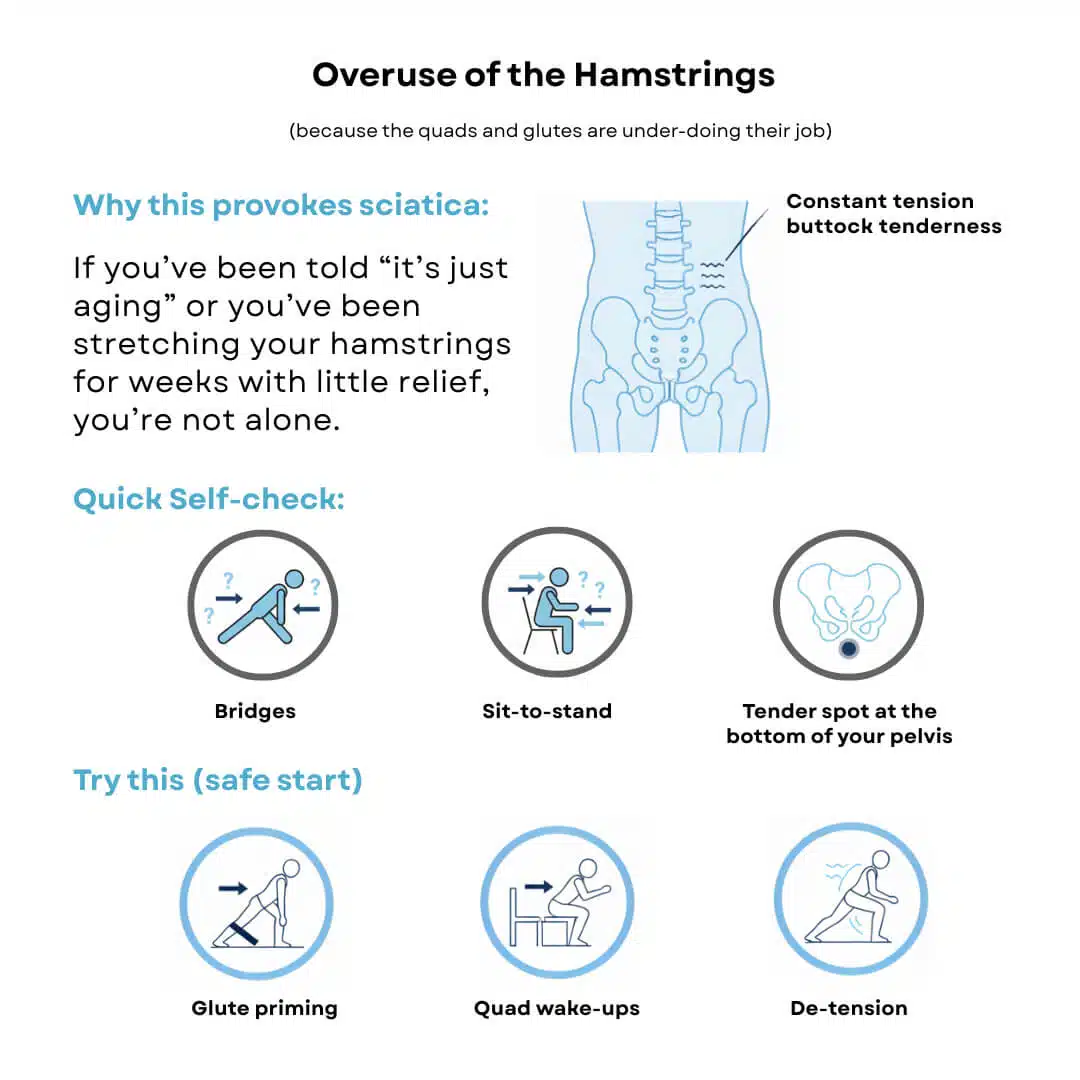
Why this provokes sciatica:
When glutes and quads check out, your hamstrings do all the lifting—especially during hinges, squats, and even standing up from a chair. That overreliance creates constant tension at the hamstring’s origin near the sit bone and along the sciatic nerve’s neighborhood. Result: buttock tenderness, “tugging” down the leg, and flare-ups after long sits or “hamstring stretches.”
Quick self-check:
- Bridges: do your hamstrings cramp before your glutes kick in?
- Sit-to-stand: do you feel it mostly in the backs of your thighs instead of your hips/quads?
- Tender spot at the bottom of your pelvis (sit bone)?
Try this (safe start):
- Glute priming: mini-band bridges (heels closer to hips), side-lying hip abduction (slow).
- Quad wake-ups: slow box squats to a chair, focus on knees tracking over the 2nd–3rd toe.
- De-tension: swap long hamstring holds for gentle nerve sliders (small, pain-free range).
2) Weak Glutes/Hips → Constant Femoral Internal Rotation
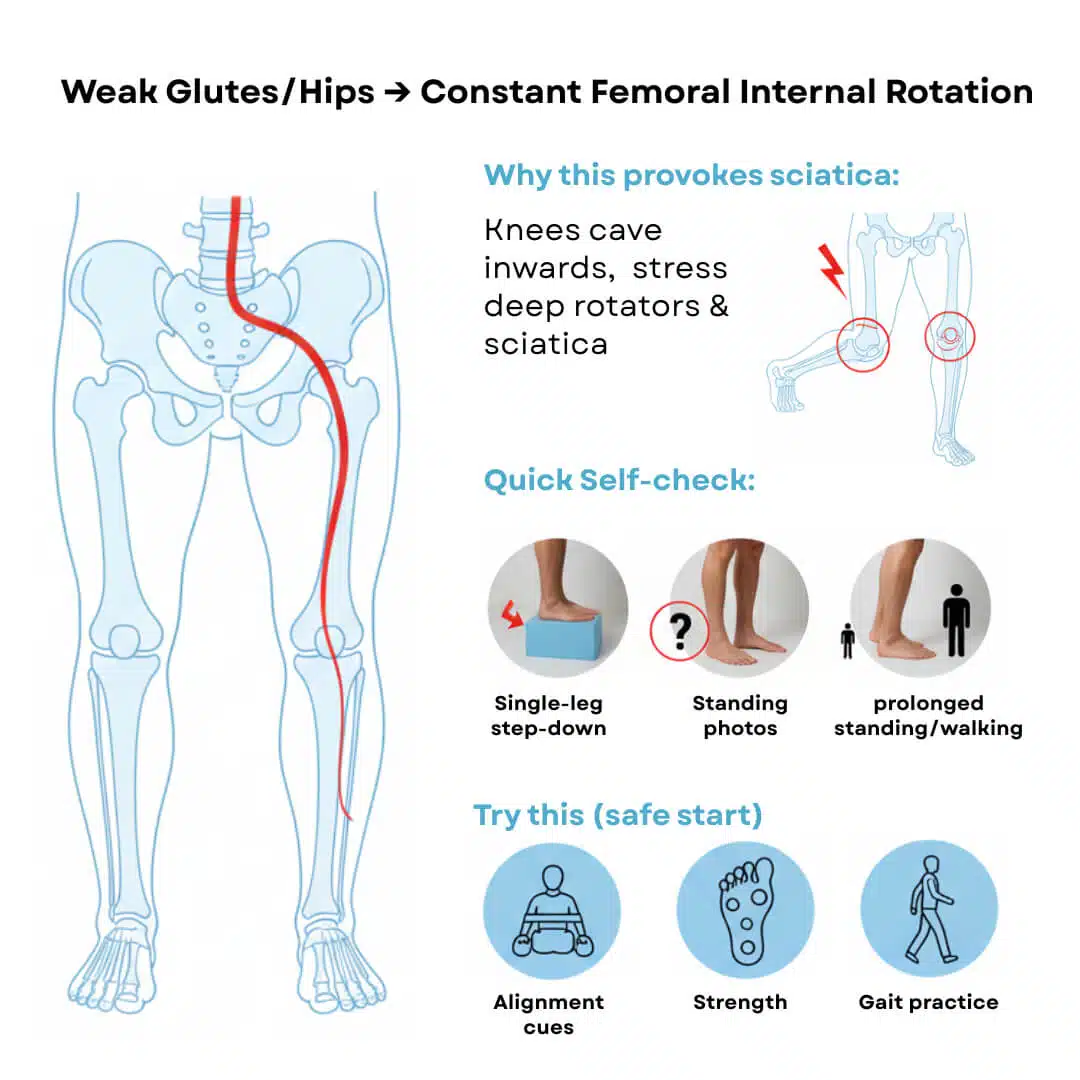
(lengthened piriformis + extra tension on the sciatic nerve)
Why this provokes sciatica:
When lateral hip stabilizers are weak, knees cave inward (dynamic valgus) and femurs live in internal rotation. That position lengthens/stresses the deep rotators (including piriformis) and can tension or irritate the sciatic nerve in the deep gluteal space.
Quick self-check:
- Single-leg step-down: do your knee and hip collapse inward?
- Standing photos: do your kneecaps point inward, arches collapse?
- Does prolonged standing/walking create a deep buttock ache?
Try this (safe start):
- Alignment cues: “knee over 2nd toe,” “tripod foot” (big toe, little toe, heel).
- Strength: clamshells (slow, band just above knees), lateral band walks, supported single-leg RDLs focusing on hip control—not weight.
- Gait practice: short walks, slow cadence, hips tall.
3) You’re Constantly Crossing Your Legs
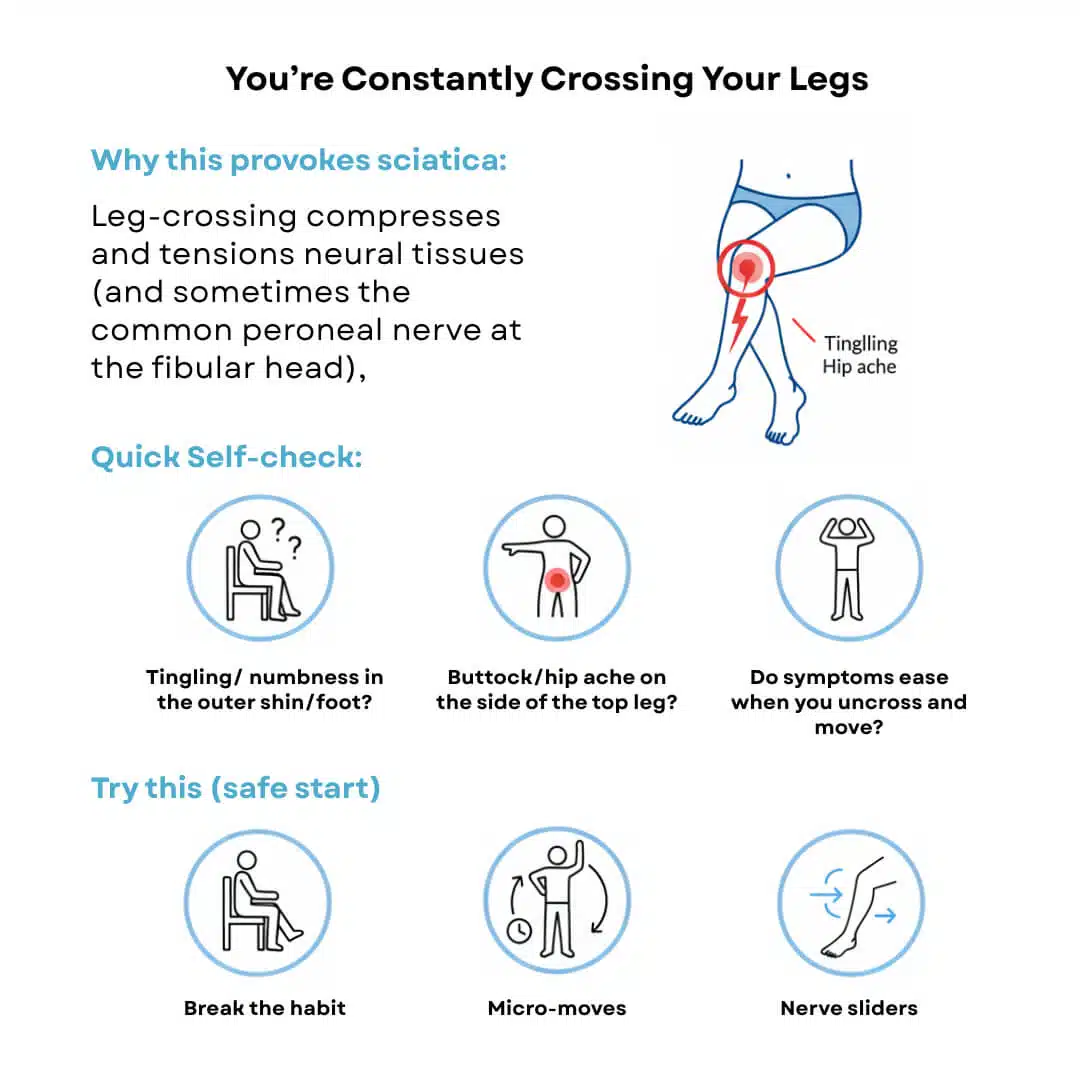
Why this provokes sciatica:
Leg-crossing compresses and tensions neural tissues (and sometimes the common peroneal nerve at the fibular head), while locking your pelvis and hip into positions that increase nerve sensitivity. Long, end-range postures are the nerve’s least favorite thing.
Quick self-check:
- Do you get tingling or numbness in the outer shin/foot after sitting cross-legged?
- Does your buttock/hip ache on the side of the top leg?
- Do symptoms ease when you uncross and move?
Try this (safe start):
- Break the habit: both feet flat or “ankle over ankle,” not knee over knee.
- Micro-moves: every 20–30 minutes, uncross, stand, and take 5–10 slow breaths.
- Nerve sliders: small, gentle reps—never into pain, never long holds.
4) You’re Sitting Too Much (and too still)
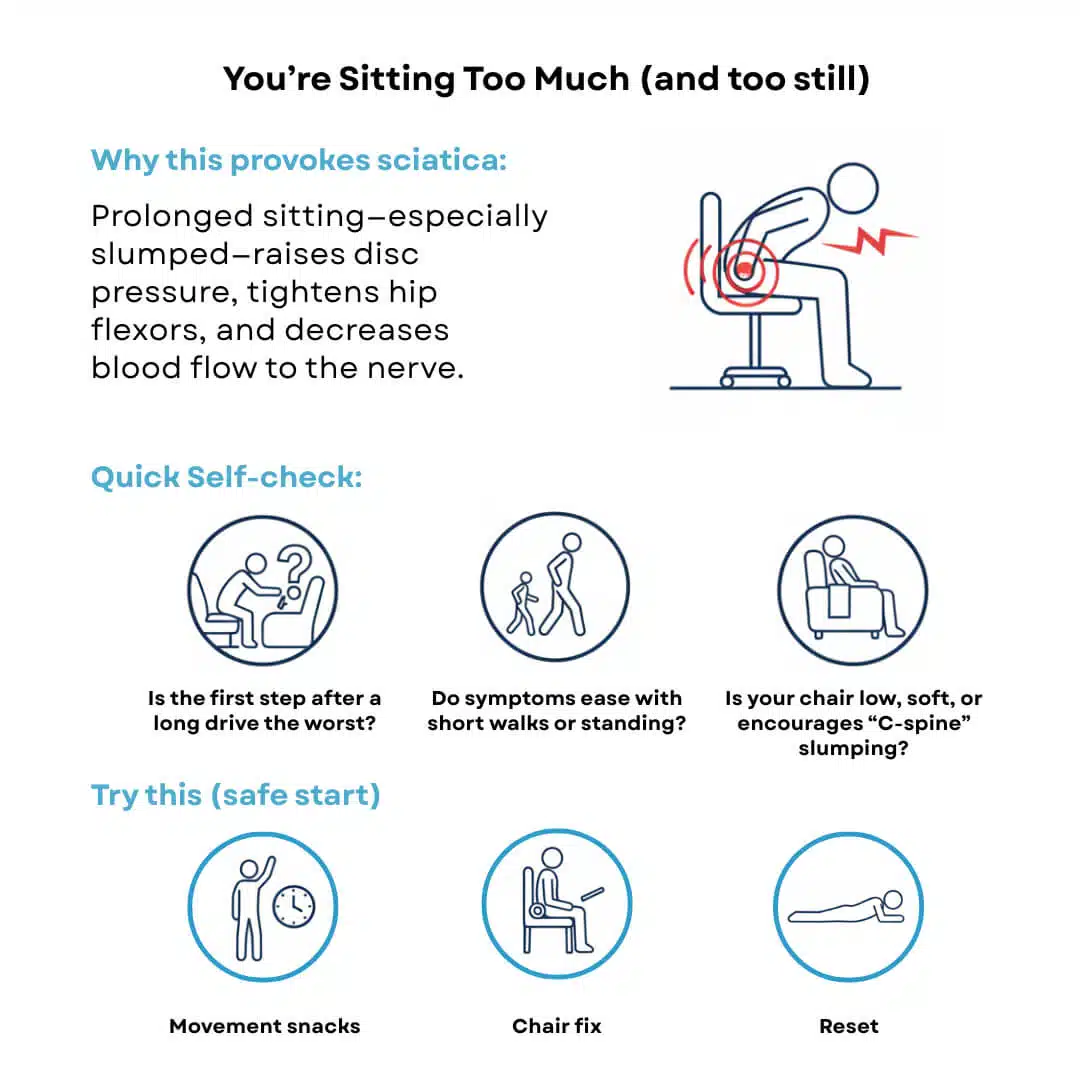
Why this provokes sciatica:
Prolonged sitting—especially slumped—raises disc pressure, tightens hip flexors, and decreases blood flow to the nerve. Nerves hate stillness; they prefer movement, variability, and space.
Quick self-check:
- Is the first step after a long drive the worst?
- Do symptoms ease with short walks or standing?
- Is your chair low, soft, or encourages “C-spine” slumping?
Try this (safe start):
- Movement snacks: set a 30–45 minute timer; stand, walk 60–90 seconds, or do 10 gentle back presses on the counter.
- Chair fix: hips slightly above knees, small lumbar support (towel roll), screen at eye level.
- Reset: 2–3 sets of prone props (on elbows) daily if comfortable.
5) A Real Tissue Irritant: Disc Herniation, SI Joint Irritation, or Hip Bursitis/Tendinitis
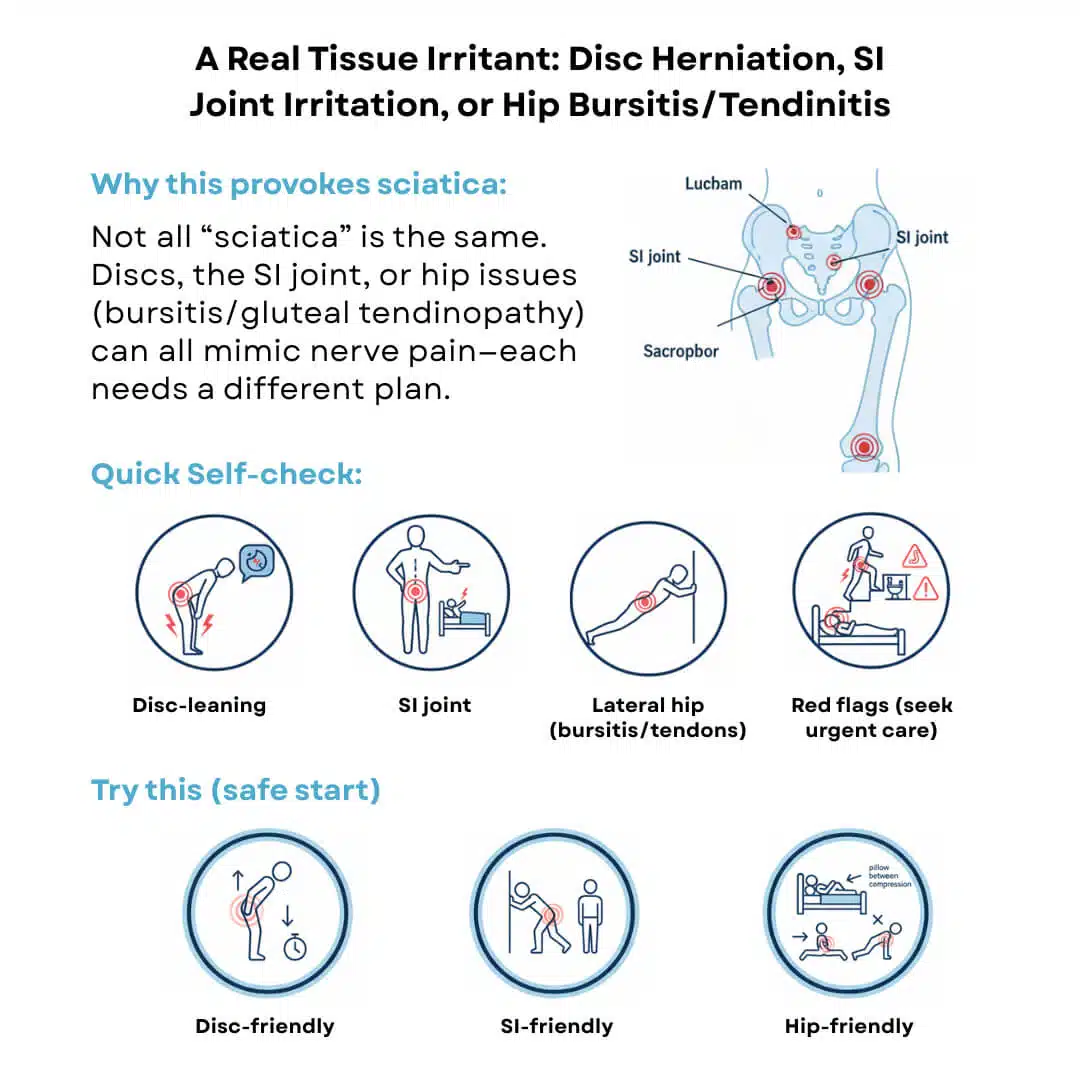
Why this provokes sciatica-like pain:
Not all “sciatica” comes from one source. A lumbar disc herniation can inflame a nerve root; a cranky sacroiliac (SI) joint can refer pain into the buttock/thigh; lateral hip bursitis or gluteal tendinopathy can mimic nerve pain with walking, stairs, or lying on your side. Each needs a slightly different game plan.
Quick self-check (clues):
- Disc-leaning: cough/sneeze or forward bending lights up the leg.
- SI joint: pain near the dimple of the low back, worse with rolling in bed or long standing.
- Lateral hip (bursitis/tendons): pain on the outside of the hip with side-lying, long walks, or stairs.
- Red flags (seek urgent care): new/worsening leg weakness, bowel/bladder changes, saddle numbness.
Try this (safe start):
- Disc-friendly: short, frequent standing breaks; gentle extension bias (if relieving).
- SI-friendly: avoid asymmetric long stands; practice tall stance and symmetrical loading; add glute med isometrics (short side-planks, wall press).
- Hip-friendly: reduce side-sleep compression (pillow between knees), start slow glute strengthening, avoid aggressive stretching early.
What Helps vs. What Hurts (Quick Rules)

Helps: frequent micro-movement, 360° breathing (exhale = ribs down), hip/T-spine mobility, anti-rotation core, loaded carries, joint-friendly strength.
Hurts: marathon sitting, leg-cross habits, aggressive toe-touch stretching early, “no pain, no gain,” random max-rep circuits.
Next Step: Fix the Pattern, Not Just the Pain
You don’t need more willpower—you need the right inputs. If these hidden drivers sound familiar, our Fixing the Cause (Not the Symptom) assessment will pinpoint your exact pattern and map a joint-smart plan you can follow with confidence.
Prefer guided coaching that respects 50+ bodies? See how we train safely and effectively on our personal trainer Fort Myers page, or call 239-223-0484 to talk with our team.
As always: this is education, not diagnosis. If symptoms escalate or you notice red flags, seek care promptly.