What Women Should Really Be Asking About Urinary Incontinence Treatment
Most women struggling with urinary incontinence ask the wrong questions.
They ask:
- “Which pad should I buy?”
- “Is surgery my only option?”
- “Aren’t bladder leaks just normal after kids or with age?”
And while these are understandable, they aren’t the right questions.
The truth is—urinary incontinence is common, but it’s not normal. It’s also highly treatable without surgery, medications, or a lifetime of pads.
In this post, I want to give you the questions you should be asking. Questions that open the door to real healing, long-term solutions, and getting your confidence back. As a women’s health physical therapist, these are the conversations I wish every woman had with her provider.
Should Ask Question #1:
“Why am I leaking in the first place?”
Most women assume bladder leaks are caused by a “weak bladder.” That’s what culture, commercials, and sometimes even doctors tell you. But the real reason isn’t your bladder—it’s your pelvic floor.
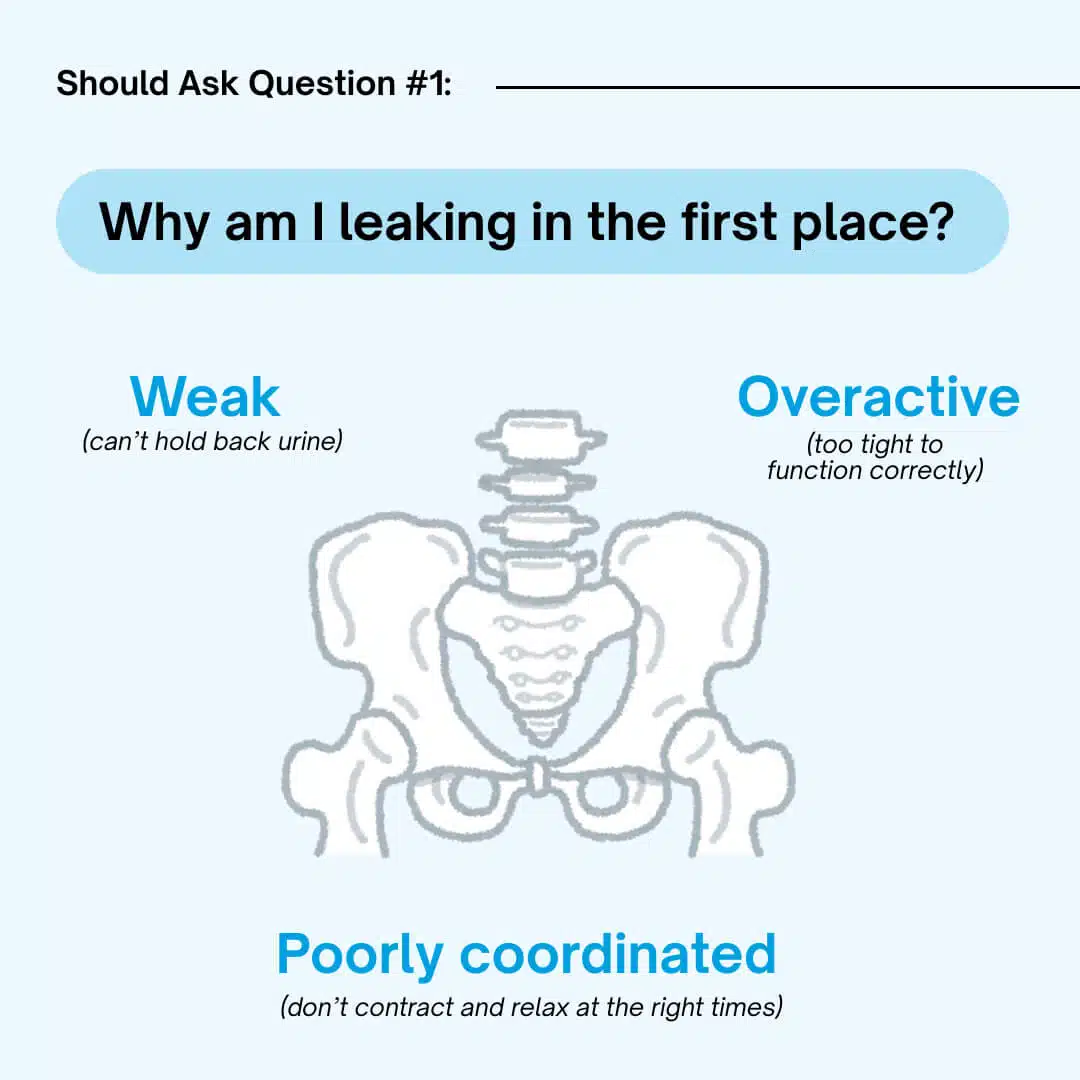
Your pelvic floor is a group of muscles at the base of your pelvis. They support your bladder, uterus, and rectum. If these muscles are:
- Weak (can’t hold back urine)
- Overactive (too tight to function correctly)
- Poorly coordinated (don’t contract and relax at the right times)
…you can end up leaking.
This is why pads and surgery don’t always solve the problem—they don’t fix muscle function. Asking “why am I leaking?” shifts the conversation from covering up symptoms to fixing the cause.
Should Ask Question #2:
“Is there a safe, natural way to fix this?”
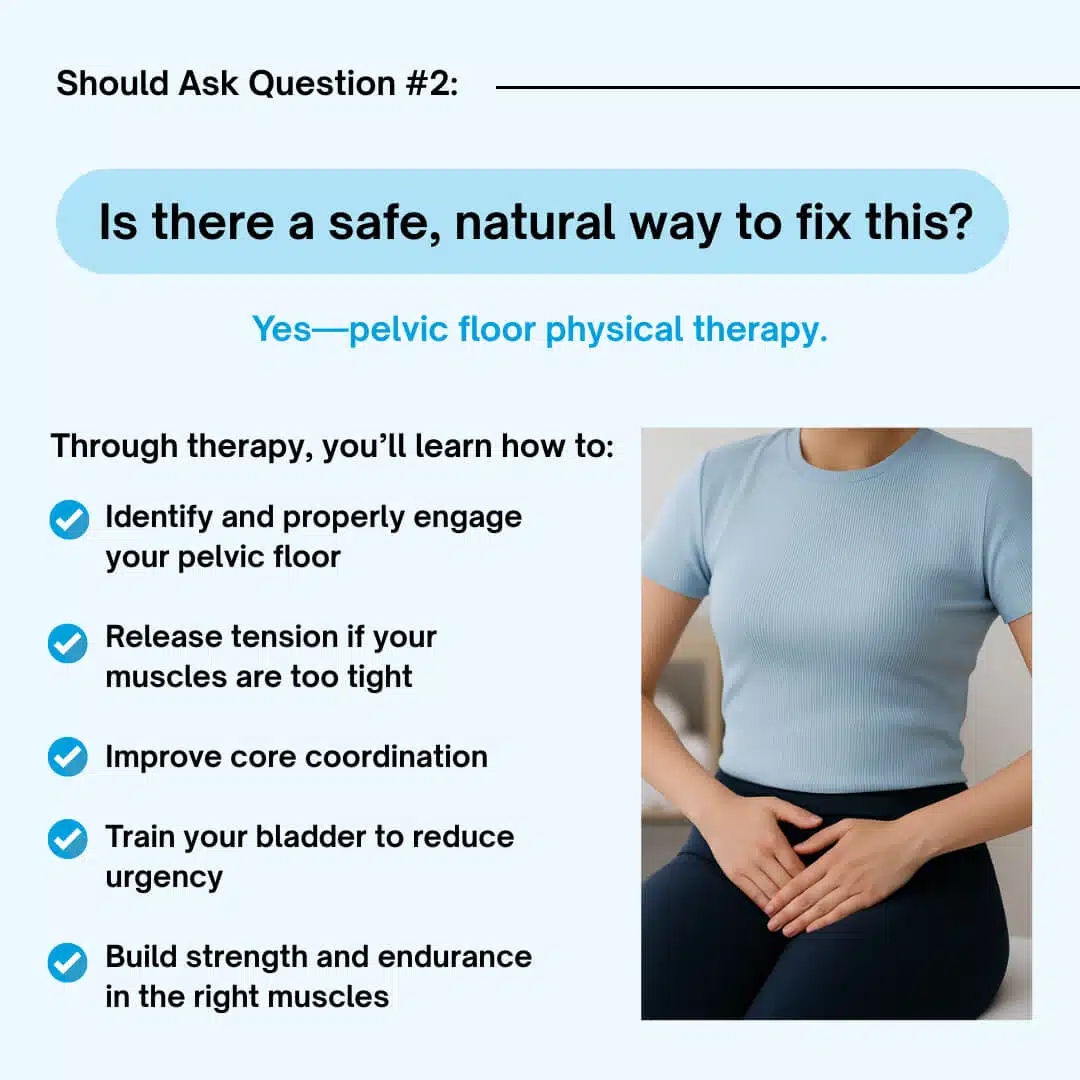
Yes—pelvic floor physical therapy.
Research shows that pelvic floor rehab is first-line treatment for most types of incontinence. In fact, studies confirm it’s just as effective (if not more) than surgery for many women, but without the risks.
- Through therapy, you’ll learn how to:
- Identify and properly engage your pelvic floor
- Release tension if your muscles are too tight
- Improve core coordination
- Train your bladder to reduce urgency
- Build strength and endurance in the right muscles
This isn’t just about doing “Kegels.” In fact, Kegels alone may make things worse if your muscles are already too tight. A skilled women’s health therapist customizes treatment based on your body’s unique needs.
Should Ask Question #3:
“What type of incontinence do I have?”
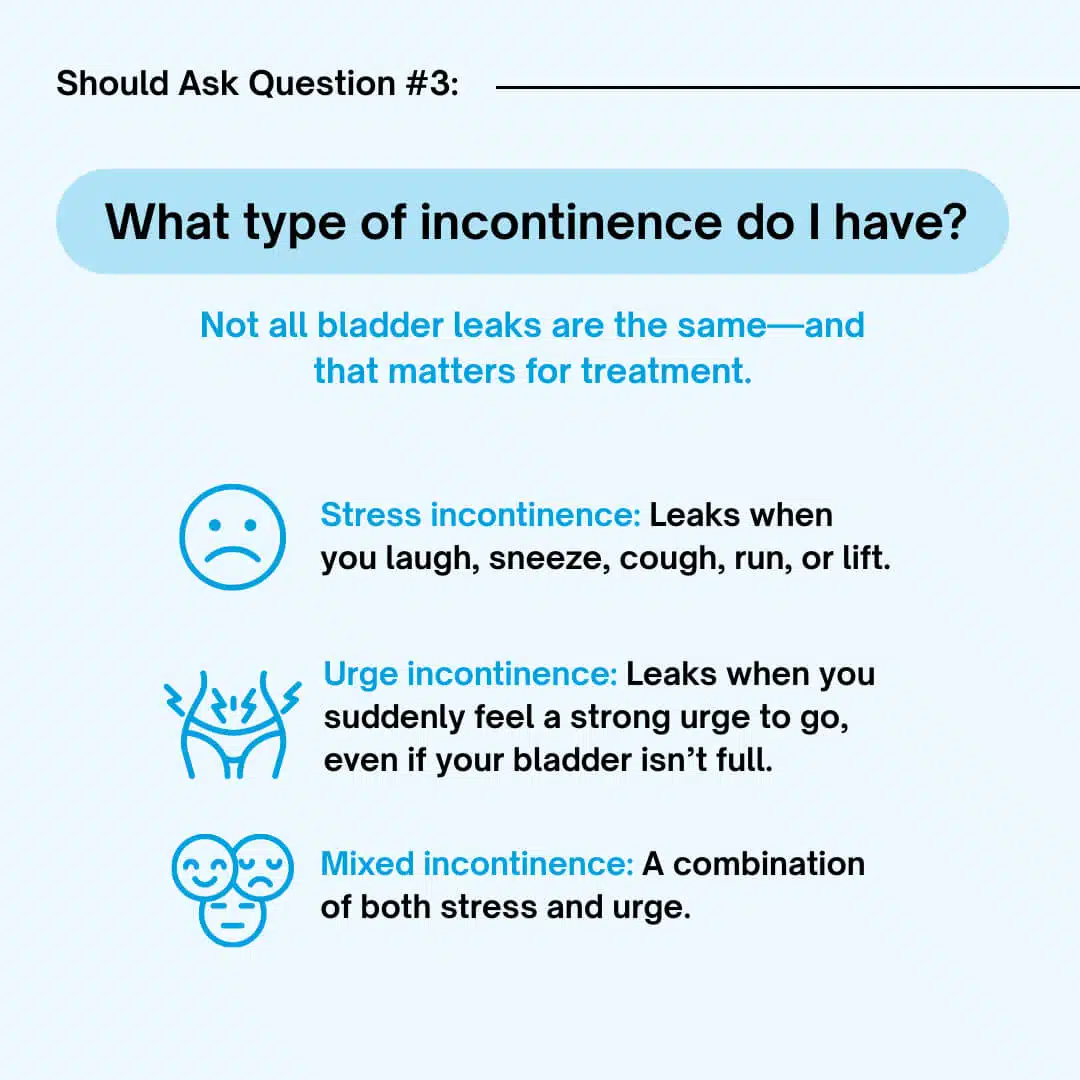
Not all bladder leaks are the same—and that matters for treatment.
The three most common types are:
- Stress incontinence: Leaks when you laugh, sneeze, cough, run, or lift.
- Urge incontinence: Leaks when you suddenly feel a strong urge to go, even if your bladder isn’t full.
- Mixed incontinence: A combination of both stress and urge.
If you don’t know which type you have, you may waste time (and money) on the wrong treatment. For example, doing endless Kegels for urge incontinence often won’t help because the issue is more about bladder signaling than muscle weakness.
A proper evaluation can tell you exactly which type you have—and what to do about it.
Should Ask Question #4:
“What’s happening in the rest of my body that might be contributing?”
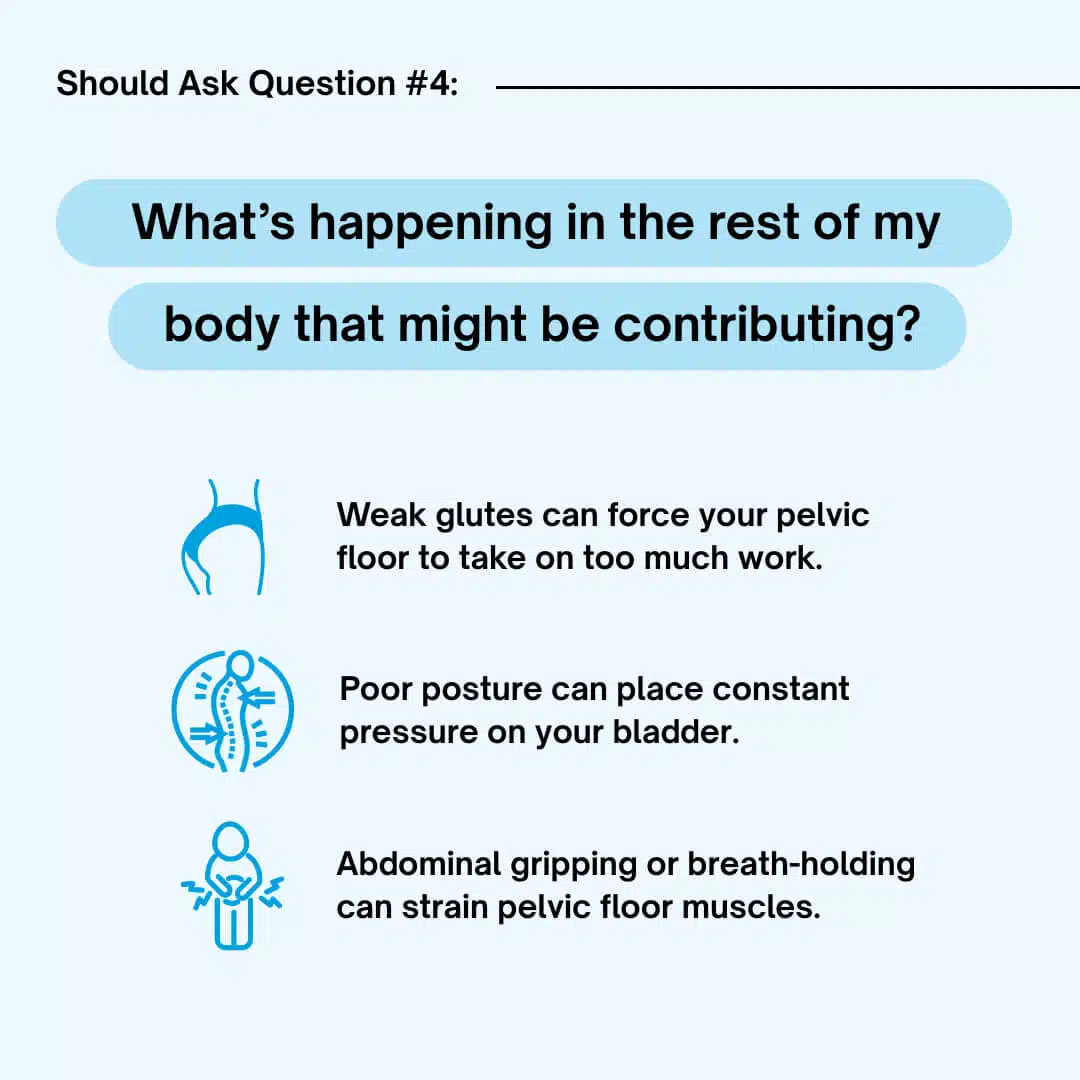
Here’s something most women never hear: incontinence isn’t always just about the pelvic floor.
Your breathing patterns, core stability, hip strength, and even posture affect bladder control. If your core and pelvic floor aren’t working together, pressure builds and causes leaks.
For example:
- Weak glutes can force your pelvic floor to take on too much work.
- Poor posture can place constant pressure on your bladder.
- Abdominal gripping or breath-holding can strain pelvic floor muscles.
This is why women’s health physical therapy looks at the whole body, not just one muscle group.
Should Ask Question #5:
“Can this really improve—even if I’ve had kids or I’m in menopause?”
Yes.
Many women think they’ve “missed their chance” if it’s been years since childbirth, or if they’re postmenopausal. But here’s the truth: your pelvic floor muscles can respond to training at any age.
- I’ve treated new moms just weeks postpartum.
- I’ve also treated grandmothers in their 70s who thought they were stuck with pads forever.
Both saw results.
The body can heal and adapt when given the right treatment.
Should Ask Question #6:
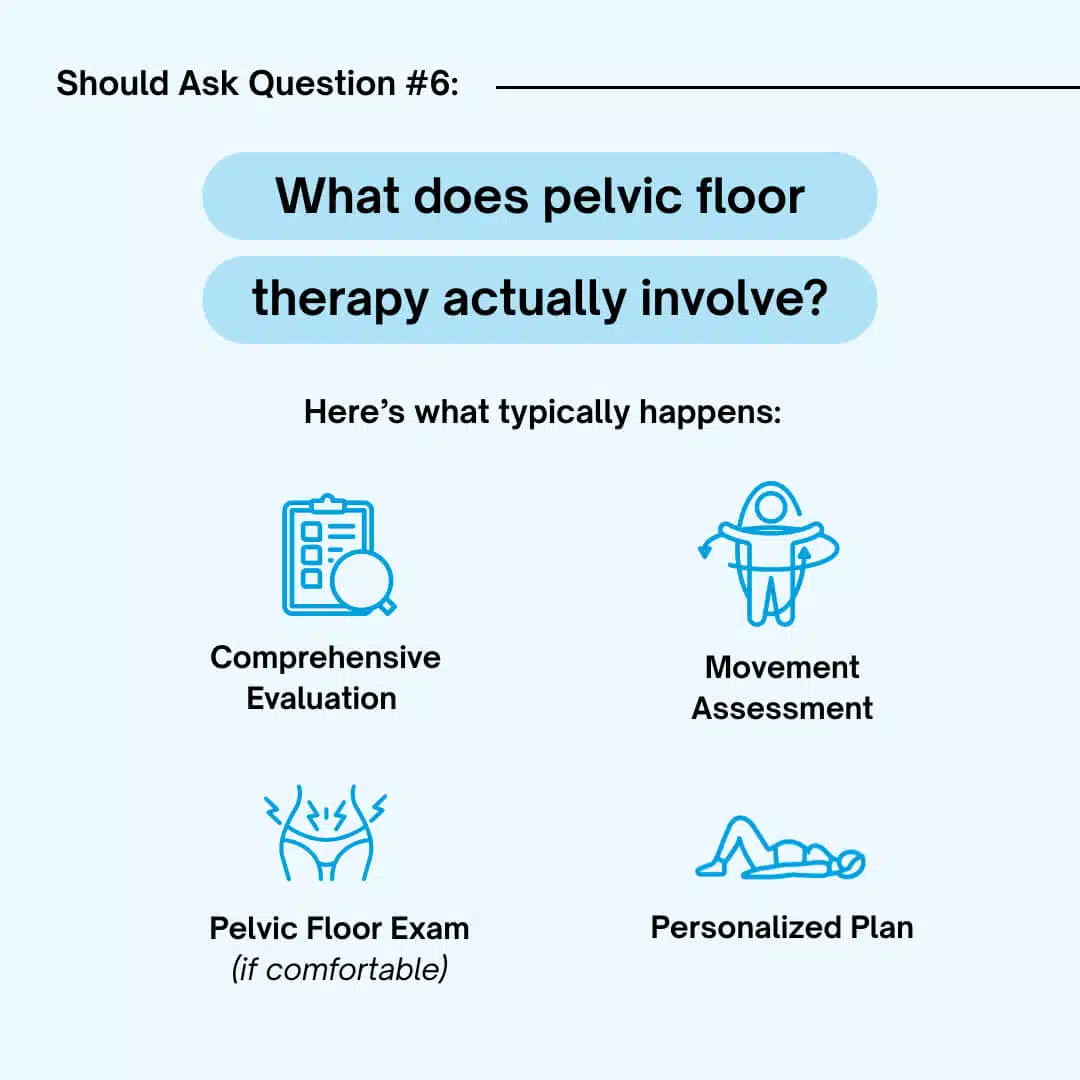
“What does pelvic floor therapy actually involve?”
This is a big one, because many women are hesitant simply because they don’t know what to expect.
Here’s what typically happens:
- Comprehensive Evaluation – We review your medical history, pregnancies, and symptoms.
- Movement Assessment – We look at how you breathe, use your core, and move in daily life.
- Pelvic Floor Exam (if comfortable) – This may involve an internal exam (similar to a gynecological exam, but less invasive) to assess your pelvic floor muscles. You’re always in control of what happens.
- Personalized Plan – We teach you exercises, strategies, and lifestyle changes to regain control.
You’re never rushed, never judged, and never pushed into anything you’re not ready for.
Should Ask Question #7:
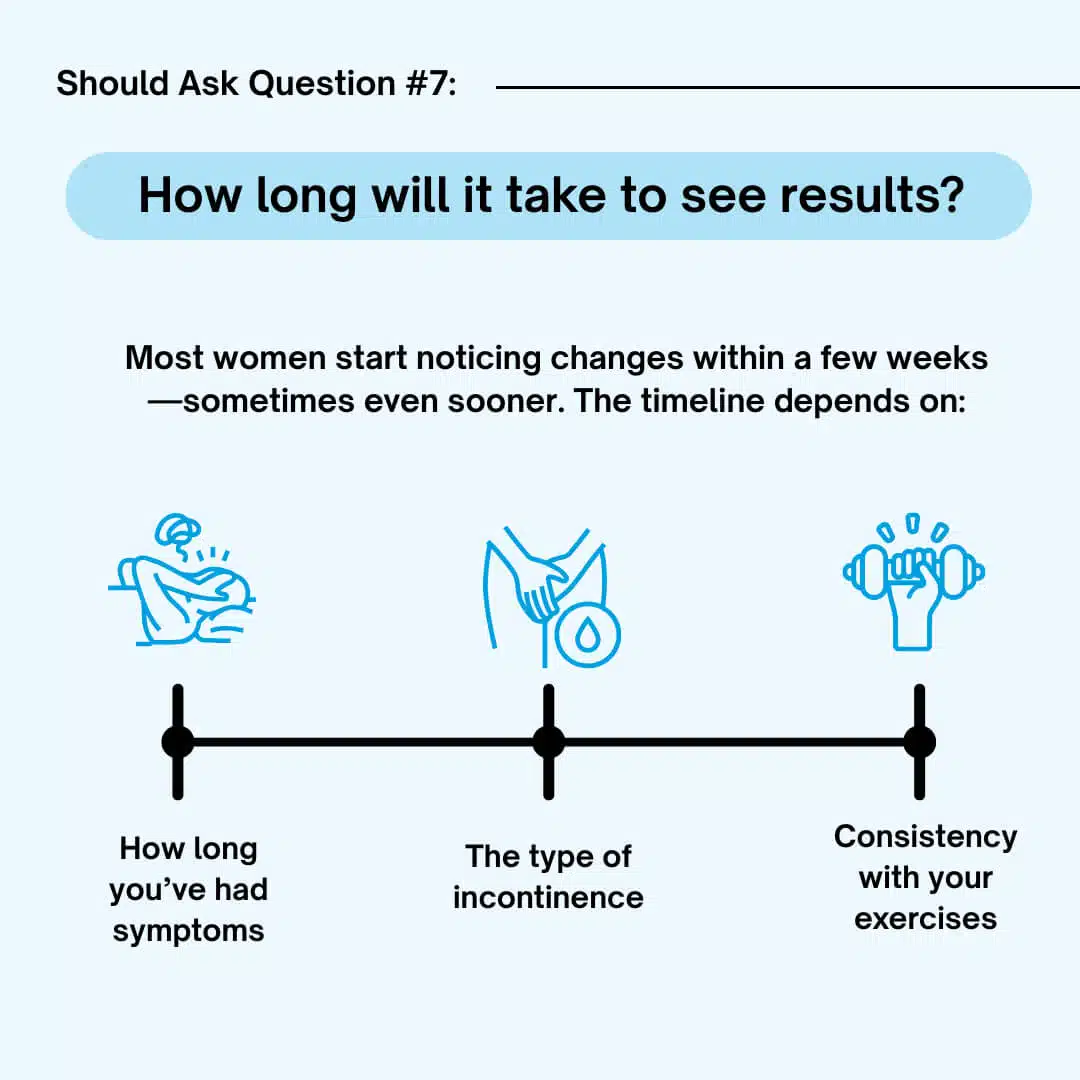
“How long will it take to see results?”
Most women start noticing changes within a few weeks—sometimes even sooner. The timeline depends on:
- How long you’ve had symptoms
- The type of incontinence
- Consistency with your exercises
On average, 6–8 weeks of dedicated therapy leads to significant improvement. And unlike quick fixes, these results are long-lasting because you’ve actually retrained your body.
Should Ask Question #8:
“What else besides exercise can help?”
Great question—because treatment isn’t one-size-fits-all.
Other helpful strategies may include:
- Bladder training: Learning how to delay urination and reset bladder signals.
- Lifestyle changes: Adjusting fluid intake, caffeine, and bowel habits.
- Breathing techniques: Restoring core and pelvic floor coordination.
- Manual therapy: Hands-on release of tight pelvic muscles or scar tissue.
For some women, we even work on hip and spine mobility, since those areas directly affect the pelvic floor.
Should Ask Question #9:
“What happens if I ignore this problem?”
This is the question that most women avoid—but it’s critical.
Ignoring incontinence often makes it worse. The pelvic floor muscles weaken further, urgency gets stronger, and leaks become more frequent. Many women who wait too long eventually face surgery or dependence on pads.
It’s not just a bladder issue—it’s a quality-of-life issue. Incontinence affects confidence, intimacy, sleep, travel, and social activities. The earlier you address it, the faster and easier it is to treat.
Should Ask Question #10:
“What’s possible if I get treatment?”
Imagine this:
- Laughing with friends without fear.
- Exercising without pads.
- Sleeping through the night.
- Traveling without planning every bathroom stop.
- Feeling confident and in control of your body again.
These aren’t unrealistic goals. I’ve seen hundreds of women go from feeling embarrassed and limited to living fully again—all because they asked the right questions and pursued the right treatment.
Should Ask Question #11:
“Why didn’t my doctor tell me this?”
This is one of the hardest truths. Many doctors still don’t refer women to pelvic floor therapy—even though research shows it should be the first line of treatment.
Why?
- Lack of training in women’s health.
- Reliance on medications or surgery.
- The misconception that leaks are “just part of aging.”
That’s why it’s so important to advocate for yourself. If your doctor hasn’t mentioned pelvic floor therapy, ask for a referral—or better yet, contact a women’s health physical therapist directly.
Should Ask Question #12:
“Where do I start?”
The best first step is a pelvic floor assessment with a trained women’s health therapist. During this visit, you’ll:
- Finally understand what’s causing your leaks
- Get clarity on whether your muscles are weak, tight, or uncoordinated
- Learn exactly what to do (and what to avoid) to fix it
- Leave with a personalized plan
The hardest part is taking that first step—but once you do, you’ll wonder why you waited so long.
Final Thoughts
Urinary incontinence is common, but it’s not your destiny. Pads, pills, and surgery are not your only options. With the right questions—and the right treatment—you can get your life back.
The next time you find yourself asking “Which pad should I buy?” or “Am I just stuck with this?”—remember to shift your focus. Ask the questions above. Demand answers that fix the cause, not just the symptoms.
And if you’re ready, know that you don’t have to walk this road alone. Pelvic floor physical therapy is safe, effective, and life-changing.
About Dr. Fernanda Paulsen
Dr. Fernanda Paulsen is a women’s health physical therapist who specializes in helping women overcome urinary incontinence, pelvic pain, and postpartum issues without surgery or medications. Her mission is to empower women to reclaim their strength, confidence, and quality of life through personalized, compassionate care.




